INTRODUCTION
Spontaneous intracranial hypotension (SIH) is caused by spontaneous cerebrospinal fluid (CSF) leakage without a history of trauma or dural puncture. Orthostatic headache is the main presentation symptom of SIH. Occasionally other symptoms may also be present, including memory loss, diplopia, nausea, neck pain, photophobia, and tinnitus [1]. Imaging techniques like brain computed tomography (CT), brain magnetic resonance imaging (MRI), spine MRI, and MRI myelography are used to diagnose SIH [2,3]. Especially, MRI myelography is an important diagnostic tool for detecting the leakage site of CSF [2–4]. SIH is often treated conservatively with hydration, bed rest, and an abdominal binder. Medical treatments, including steroids, acetazolamide, and intravenous caffeine, have been tried [5]. It has been found that only 37% of patients treated with conservative measures reported headache relief at 6 months, and the actual efficacy and optimal duration of bed rest have not been proven [1]. Epidural blood patch (EBP) is the most commonly performed, especially following failure of conservative management [1–3].
We reported a case in which a patient with SIH was treated with an EBP under fluoroscopic guidance.
CASE REPORT
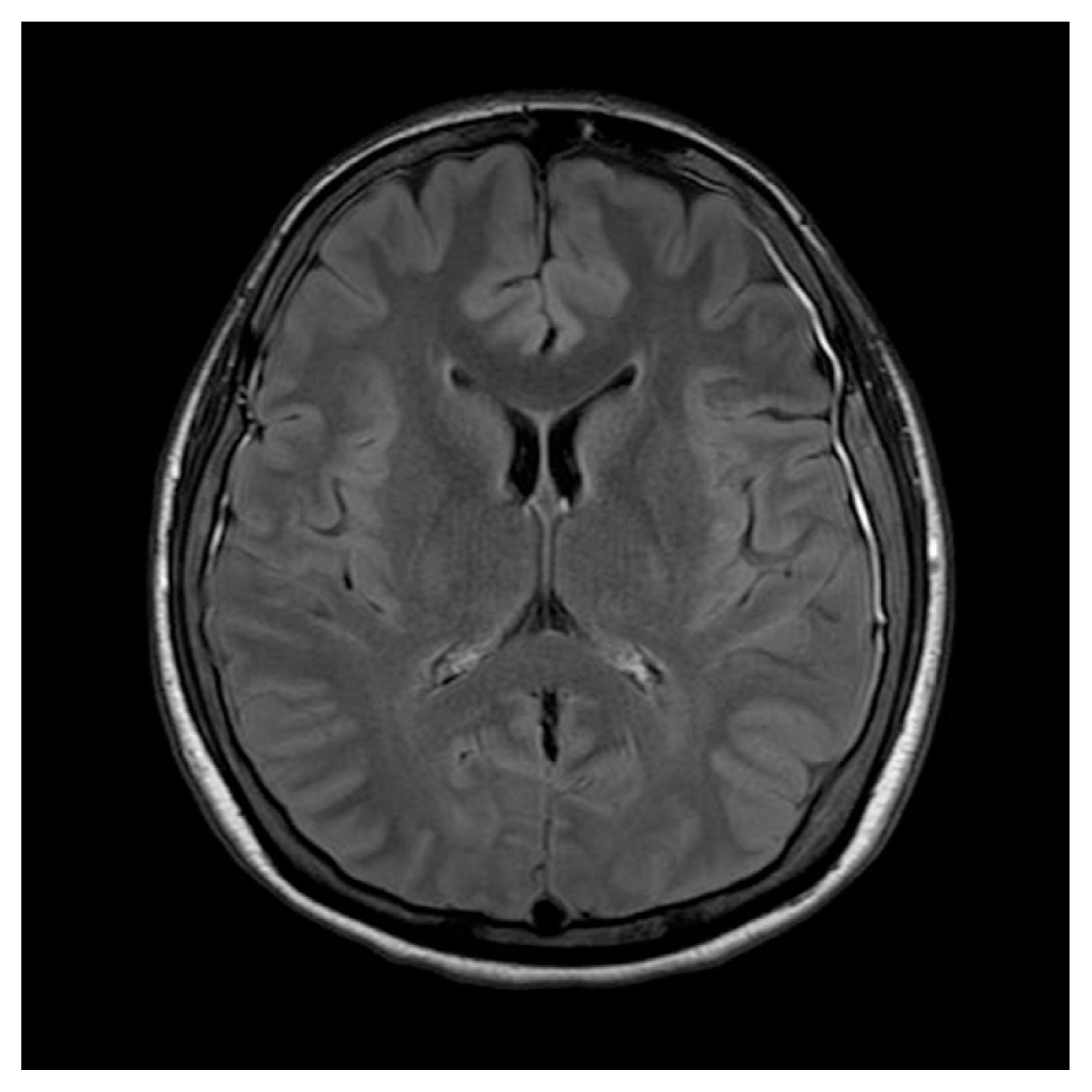
A 32-year-old woman presented to the emergency room of Samsung Changwon Hospital with a severe headache, nausea, and vomiting. The headache worsened when sitting or standing and partially regressed when lying down. The initial headache was a severe pain that she had never experienced, and the Visual Analog Scale (VAS) at this time was about 6–8. She had a history of treating symptoms using painkillers for migraine for several years. She had no trauma history, no relevant family history, and showed no neurologic signs. An emergency medical doctor performed a lumbar puncture and CSF pressure was found to be 7 mm Hg. CSF analysis revealed no abnormal findings. Brain CT was performed and no specific findings were found. Brain MRI showed typical signs of intracranial hypotension with diffuse pachymeningeal thickening (Fig. 1). SIH was suspected clinically symptoms and she was admitted to the neurology department.
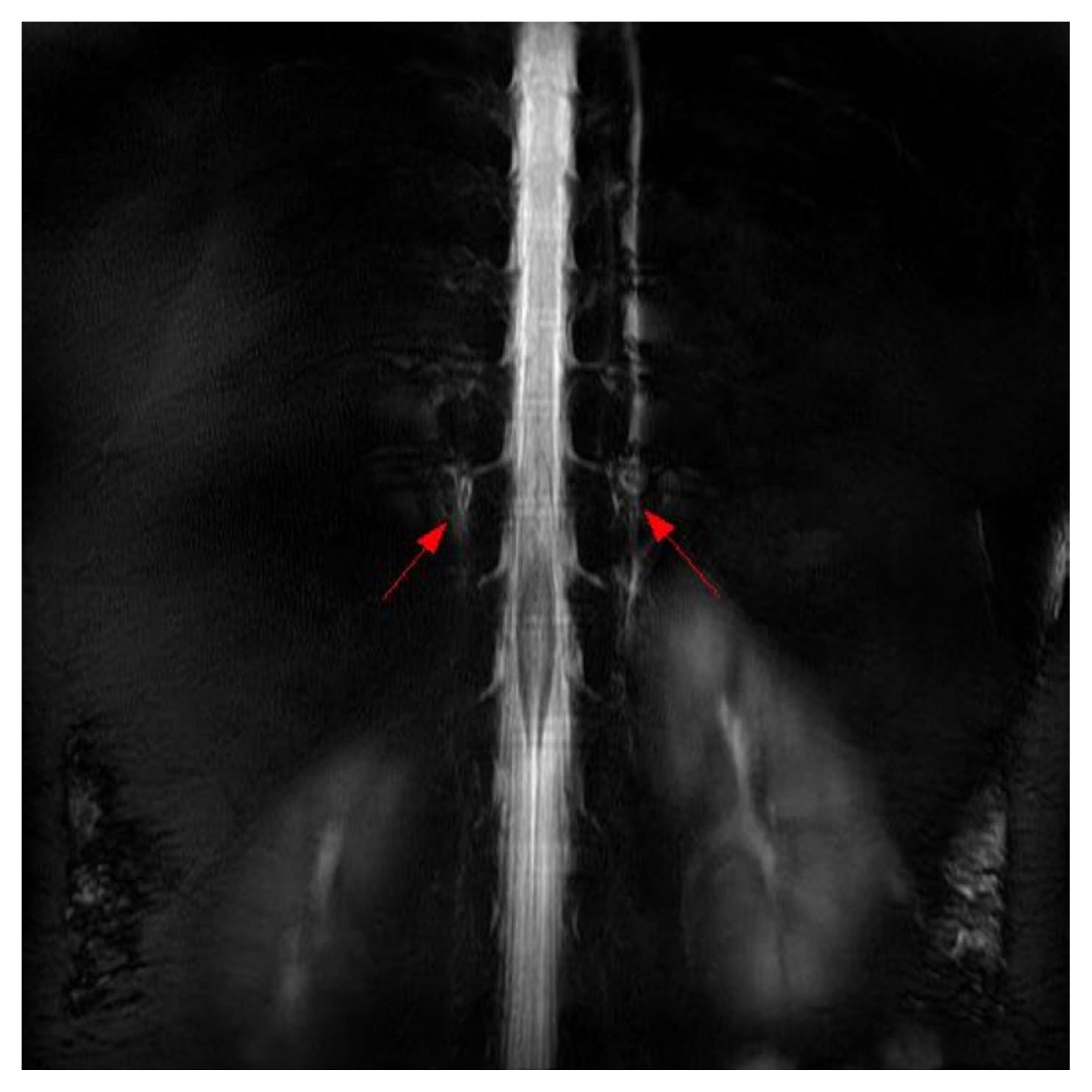
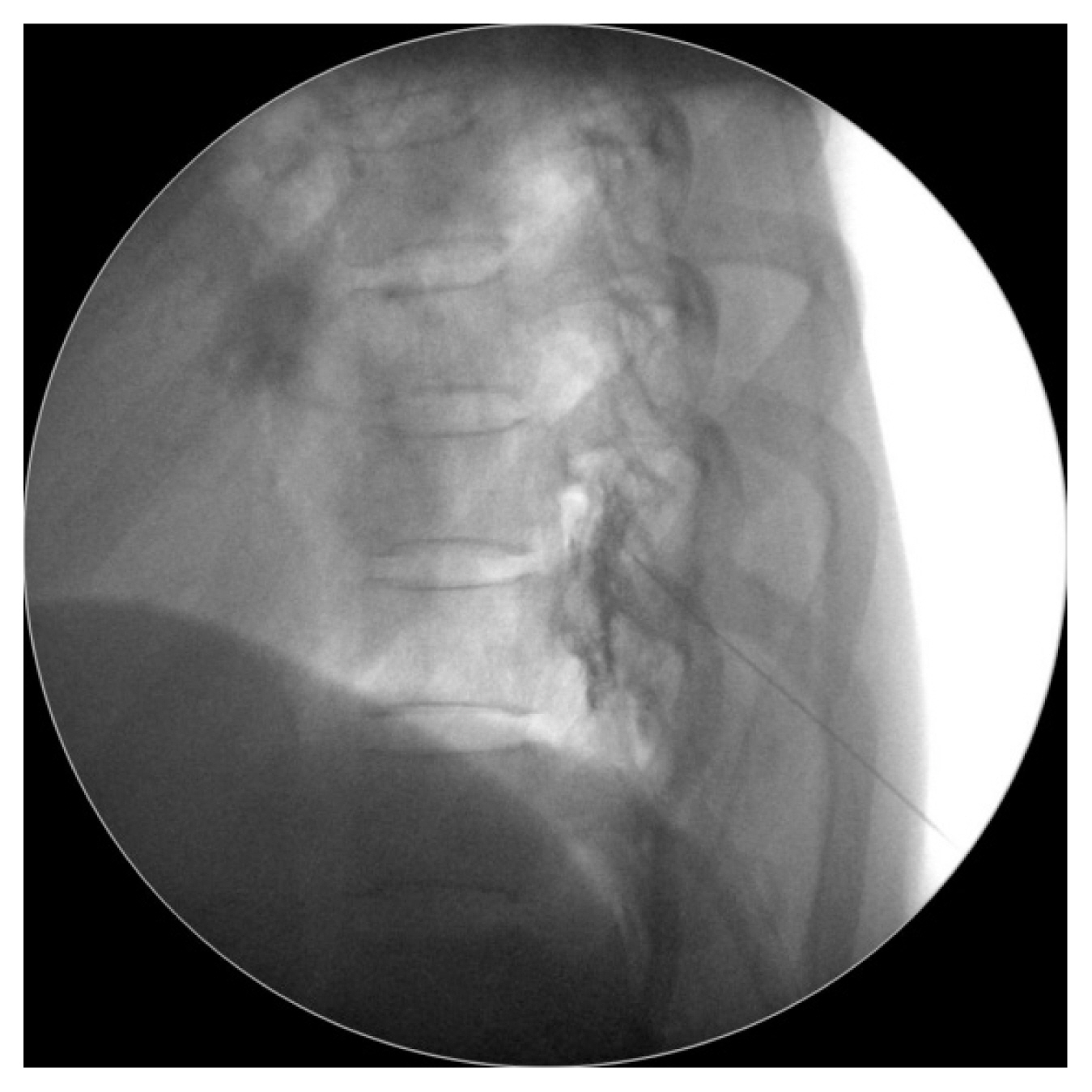
She was treated with conservative treatment, including bed rest, intravenous fluid administration, and analgesics. EBP treatment was considered and the patient wanted to receive this treatment. The patient was referred to our pain clinic with a diagnosis of SIH and we performed a blind EBP at a lumber spine level. The EBP was performed under the guidance of fluoroscopy using a contrast agent and 15 mL of autologous blood at the L4–5 level (Fig. 2). The headache improved after the procedure (from VAS 4 to 2) but, on the second day after the procedure, the pain worsened again. We performed an MRI of the spine and magnetic resonance myelography to identify the site of CSF. It shows ill-defined fluid collection at the anterior and posterior epidural space on the entire spine level and CSF accumulation on the retrospinal C1–2. It revealed CSF leakage from the C-T spine junction and lower T spine level (Fig. 3).
The patient agreed to undergo EBP therapy at the thoracic level. In the pain clinic, a 22G Tuohy needle was inserted into the middle epidural space at the T9–10 level. A total of 24 mL of autologous blood was injected (Fig. 4). The injection resulted in an improvement in the headache (from VAS 4 to 2) at the pain clinic. In the ward, she complained of upper back pain, but her headache showed improvement. Five days later, her headache was almost resolved, and she was discharged. Written informed consent was obtained from our patient for the publication of this report.
DISCUSSION
SIH is a disorder of low CSF volume and pressure (less than 60 mmH2O) caused by persistent CSF leakage through a dural defect in patients without a previous history of trauma or dural puncture [3–5]. Although there are no universally accepted diagnostic criteria for SIH, the diagnosis of SIH is dependent on clinical history, neurologic examinations, imaging studies, and CSF studies [4]. Neuroimaging techniques used in the diagnostic process may be cranial, to assess the consequences of CSF hypotension, or spinal, to localize the leakage and possibly guide diagnosis if a targeted treatment is pursued [1]. MR myelography is the most common noninvasive method for detecting the site of a CSF leak, which can show pachymeningeal enhancement, extradural fluid extravasation extending to the paraspinal space, and engorgement of epidural venous plexuses [1–4].
Autologous EBP is considered to be the treatment of choice for patients who have failed initial conservative treatment. The mechanism of the blood patch is thought to be due to the covering of the meningeal tear site with a blood clot [5]. Shima et al. [4] reported that autologous EBP was effective in 48% of patients who could not be treated effectively with initial conservative treatment. Many studies have suggested the technical details of EBP [3–10]. However, the response rate to initial EBP varies significantly among reports, ranging from 36% to 90% [9]. Signorelli et al. [9] performed a systematic review and meta-analysis of the existing literature to find out the roles of different factors that can affect the efficacy of the EBP procedure. Among the factors analyzed, none was found to be statistically significant in affecting the efficacy of the EBP procedure [9]. Yoon et al. [11] and Choi et al. [12] reported the distribution of blind versus targeted EBP in responders and non-responders. Neither found significant differences between the two groups.
EBP is less invasive than surgical repair of the CSF leakage, but variability remains concerning the volume of injected blood and technique, being performed as a targeted patch if the leaking site is known or as a non-targeted (blind) patch. Blind EBP is an approach in which the patch is delivered to the lumbar or thoracic spine, away from the site of leakage, without the need for radiologic imaging [7]. Also, empirically two-level patching is performed [5,7]. The use of blind EBP eliminates the additional radiation exposure, provides an opportunity for immediate treatment, and allows for blood administration via the lumbar route, which is a relatively wide and safe approach [10]. Ferrante et al. [10] demonstrated that a patient with SIH, due to an upper cervical CSF leakage, could be successfully treated with an autologous lumber EBP at the L2–3 level. Some authors have reported that targeted EBP may be more successful than non-targeted patching [11,13]. A lower proportion of patients initially treated with targeted EBP required repeat EBP compared with those initially treated with blind EBP. These findings are consistent with previous studies that demonstrate the superior efficacy of targeted EBP versus blind EBP.
There have been reported cases of successful treatment using bilevel EBP in patients where the site of CSF leakage was not clearly identified on imaging [5], or in patients with multilevel CSF leakage seen on imaging [6]. Interestingly, there is a study that investigated the effectiveness of initial two-site blind EBP, which involves the administration of EBP at the cervicothoracic and thoracolumbar levels to effectively span the entire spinal column. They observed similar outcomes after the initial two-site blind EBP and targeted EBP. And, they suggested, two-site blind EBP is an effective alternative to conventional targeted EBP and a potential initial patch of choice for SIH treatment [14].
SIH is typically caused by a CSF leak, leading to an overall decrease in CSF volume. This can cause brain sagging with traction and distortion of the central nervous system and surrounding structures leading to the primary symptom of postural headaches [15]. This condition may lead to other complications as severe as the development of subdural hematomas (SDH). Although, management of SDH arising in the setting of SIH still lacks consensus. However, prompt identification of SIH and early treatment of CSF leak can prevent complications from occurring, including SDH formation. In the case of the development of symptomatic SDH, both an EBP and surgical evacuation of SDH may be necessary. Careful attention to the nature of the patient’s headache is needed to distinguish a low-pressure state in SIH versus a high-pressure state from a symptomatic SDH [3,15].
The success rates for EBP have been shown to increase with the volume of blood, with a rate of 80% achieved with 10–15 mL and >95% with 20 mL [3,7,14]. But some reported a targeted EBP with a small volume of blood can be used with good effect [5,8,13].
In conclusion, this report describes the treatment of SIH with targeted EBP according to imaging diagnosis after the failure of initial blind lumbar EBP. In addition to targeted EBP treatment, we would like to recommend that two-site blind EBP be considered as an initial treatment method. We believe that more studies and cases are needed for this.