INTRODUCTION
An Imperforate hymen is a congenital disorder where a hymen without an opening obstructs the vagina. The symptoms of imperforate hymen come from distended uterus and vagina with a large amount of menstrual blood after puberty [1,2]. It is the most common congenital anomaly of distal female genital tract obstruction, but it has a low incidence, of only 1/16,000–30,000 in newborns [3]. Imperforate hymen with urinary retention is even more rare. Most symptoms of imperforate hymen occur because of the accumulation of menstrual blood after puberty. It can rarely be found before puberty. Periodic abdominal pain and discomfort of the pelvic region are most commonly observed, and these symptoms increase with bowel movement before puberty. If the menstruation begins after puberty, continuous accumulation of menstrual blood leads to vaginal hematoma or even to hysterovaginal, ovarian, or abdominal hematomas. Rarely, compression of the surrounding tissues can result in voiding difficulty such as dysuria, frequent urination, or oliguria.
We experienced a rare case of imperforate hymen with urinary retention. Here, we report on this case with a brief review of the literature.
CASE REPORT
A 13-year-old girl had not defecated for 10 days. She tried to urinate but failed to. She visited a clinic several times and got an enema. She had severe constipation because she does not move much. There were no specific findings in the medication and disease history that could affect a voiding symptom. But she had no menstruation. She did not urinate well, had a strain to void, and felt residual urine sensation. We checked the residual urine volume with BladderScan (model BVI 3000; Verathon, Bothell, WA, USA) at the time of admission and the residual urine volume was 1,000 mL. Foley catheterization was performed. When the Foley catheter was inserted, a large vaginal mass was seen in the hymen. She had developed breasts and pubic hair according to her age. A vaginal exam was performed, and the pelvic mass was touched (Fig. 1).
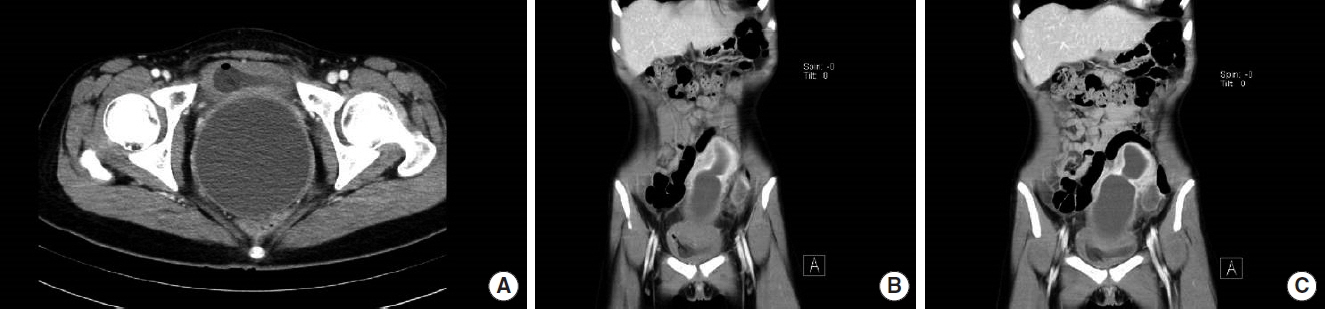
Complete blood count, white blood cell, hemoglobin, hematocrit level, and urinalyses revealed no specific finding. Hydrometra was found on a computed tomogram scan (Fig. 2). The uterus had a large amount of fluid in the upper pelvic cavity. She was referred to our obstetrics and gynecology outpatient clinic. Hymenoplasty was performed under general anesthesia and about 800 mL of blood was evacuated. The next day she had no voiding symptom. The residual urine volume was 0 mL. After operation, all of symptoms with voiding symptom were improved.
DISCUSSION
Failure of hymen perforation is a rare hereditary anomaly. The incidence of imperforate hymen is very low, between 1/16,000–30,000 [3]. Imperforate hymen, transverse vaginal septum, and vaginal atresia with or without persistence of a urogenital sinus of cloaca are common causes of secretory hydrometrocolpos [1,2]. Embryologically, two mullerian ducts fuse, and form a single uterovaginal canal at around 8–10 weeks [1,2,4]. The vagina is developed from uterovaginal canal and sinovaginal bulb [1,2,5]. Complete patent vagina is formed around the 5th month of gestation [2]. The vagina has six different developmental phases [4]. Hymen development has a dual origin from the sinovaginal bulb and urogenital sinus cavity and vestibule [1,2]. Embryological defects can occur during development, differentiation, migration, apoptosis, fusion, and canalization [5]. Vaginal atresia with hydrometrocolpos may be a part of complex syndromic anomalies, which include Mckusick-Kaufman syndrome and Bardet-Biedl syndrome [1,2,6]. Imperforate hymen is a local fusion anomaly with defective resorption of the mullerian septum [1,2,5]. The development of mesonephric and paramesonephric ducts is interdependent, and their paracrine actions also have a role in hymen development. Hymen anomalies may present with concomitant anomalies of the above three structures [2,7,8]. Hymen perforation occurs commonly during fetal life or the perinatal period [1,2].
Most symptoms are caused by the accumulation of menstrual blood after puberty and so rarely occur before puberty. Periodic discomfort and pain of lower abdomen and pelvis are the most commonly observed symptoms, and these increase during defecation [1,2]. The diagnosis can be made by symptoms and physical findings including a mass in the upper part of the pubic bone or a soft and rounded mass protruding because of the tension of the vulva on the pelvic examination. After punctation, the fluid was drained and the mass disappeared [9,10]. This case can be diagnosed by a protruding mass in the hymen and a hydrometra in the computed tomography photograph.
The differential diagnosis is uncommonly an ovarian, enteric duplication, mesenteric, choledochal, adrenal, urachal, or splenic cyst, meconium pseudocyst, cystic renal masses, anterior sacral meningocele, inter-abdominal cystic variety of sacrococcygeal teratoma, and chylous ascites [3].
Before puberty, the treatment of imperforate hymen is done with a crescent-shaped incision or a simple incision at 2, 4, 8, and 10 o’clock. After puberty, a simple cross-incision is made after the puncture. Antibiotics are needed before and after surgery [11–13]. In this case, after puberty, a simple cross-cut was made after puncture, and antibiotics were used before and after the operation.
For simple vaginal hematoma the prognosis is good, and the function of the reproductive tract returns quickly. The vagina, uterus, and fallopian tubes have great powers of regeneration despite dilatation. Bilateral changes of the salpinx develop infertility [14].
Our case was easily diagnosed in obstetrics and gynecology, but it is not easy to diagnose in urology. Especially, if the urologists concentrate on the urination only, they may miss it. When girls without menstruation cannot urinate, the vaginal exam can help.