The Predictive Factor for Favorable Outcome after Surgical Treatment of Benign Prostate Hyperplasia Performed by Young Urologist: Is Surgical Modality Important in Beginner Urologists?
Article information
Abstract
Objective
To identify predictive factors for favorable outcomes after surgical treatments that were performed by beginner urologists in patients with benign prostate hyperplasia (BPH), we retrospectively evaluated outcomes after holmium laser enucleation of the prostate (HoLEP) and transurethral resection of prostate (TURP) that were performed by two young urologists.
Methods
Of 80 patients who were treated with HoLEP or TURP, 31 (HoLEP) and 36 (TURP) patients who were followed up for 3 months were enrolled in this study. Preoperative and perioperative variables were evaluated to identify predictive factors for favorable outcome after surgical treatment for BPH.
Results
At 3 months postoperative after HoLEP or TURP, the median decrease in International Prostate Symptom Score (IPSS) was 13.0. Patients whose IPSS decreased by over 13 points were categorized into a favorable response group after HoLEP or TURP. Univariate and multivariate logistic regression analyses were performed to identify predictors of favorable outcomes at 3 months after HoLEP or TURP, and the preoperative IPSS was identified as an independent predictor for favorable outcomes.
Conclusion
When young urologists plan to perform surgical treatment for BPH, they should consider that the severity of symptoms is the most important factor for favorable outcomes. The type of surgical modality for managing BPH is less important.
INTRODUCTION
Transurethral resection of prostate (TURP) has been the gold standard for surgical treatment of lower urinary tract symptoms due to benign prostate hyperplasia (BPH) [1]. However, since holmium laser enucleation of the prostate (HoLEP) was introduced as the treatment for benign prostatic hyperplasia (BPH) [2], several clinicians have suggested that HoLEP could replace TURP as the current gold standard for the treatment of BPH [3].
While it has been reported that HoLEP is an admirable challenger of TURP [4,5], several clinicians hesitate to perform HoLEP because of its steep learning curve [6–11]. In addition, most young beginner urologists agonize over selecting HoLEP as a surgical modality for BPH, because most previous reports on the learning curve associated with HoLEP included only expert surgeons. To the best of our knowledge, there is no comparative study in younger urologists regarding their learning curve for TURP and HoLEP. For this reason, the factors that should be considered for proper patient selection and surgical modality should be determined for young beginner urologists who decide to perform surgical treatment for BPH.
Authors have attempted to identify predictive factors for favorable outcome after HoLEP and TURP that were performed by young beginner urologists in BPH, and tried to investigate whether surgical modality is an important factor.
MATERIALS AND METHODS
1. Procedure
Two young urologists performed surgical treatment for BPH after completing fellowship training for 2 years. HJY performed only HoLEP as the modality for surgical treatment of BPH, and KHK performed only TURP in all cases.
A 72-W OmniPulse (Trimedyne Inc., Irvine, CA, USA) was used for the HoLEP, and the energy source consisted of a 72-W holmium: yttrium aluminum garnet laser with a 550-μm laser fiber. Enucleated prostatic tissue was removed using transurethral morcellation by use of a mechanical morcellator (Richard Wolf, Knittlingen, Germany) that was introduced through an offset rigid nephroscope. In cases of TURP, a standard Richard Wolf rectoscope and working elements were used, and a bipolar technique was applied in all TURP cases.
2. Patients
Forty consecutive patients who were treated with HoLEP by H.J.Y. and TURP by K.H.K. for BPH were included in this study. HoLEP cases were performed between June 2014 and November 2016, and TURP cases were performed between April 2016 and March 2017. Of 80 patients who were treated with HoLEP or TURP, 31 (HoLEP) and 36 (TURP) patients who were followed up to 3 months were enrolled in this study. After receiving institutional review board approval (IRB approval no., 2017-07-022), we conducted a retrospective chart review of 31 (HoLEP) and 36 (TURP) patients. The requirement for informed consent from individual patients was omitted because of the retrospective design of this study.
3. Clinical data and statistical analysis
Age at time of surgery, body mass index, surgical modality for BPH, medical history, preoperative prostate specific antigen (PSA), International Prostate Symptom Score (IPSS), quality of life (QoL) score, the maximum urinary flow rate (Qmax), post-void residual urine volume, total prostate volume, transition zone volume, and history of acute urinary retention were estimated as preoperative variables for analysis, and weight of resected tissue, operative time, volume of resected tissue, resection speed, resected ratio, catheterization duration, and hospital days were used as perioperative variables. Resection speed was defined as the total amount of removed tissue after TURP or HoLEP in gm divided by total operative time in minutes [12], and resected ratio was defined as volume of resected tissue divided by preoperative transition zone volume. Serum PSA for all included patients was assayed with a Cobas-e411 system (Roche Diagnostics, Rotkreuz, Switzerland), and prostate volume and transition-zone volume were estimated from transrectal ultrasound (TRUS) results using the prolate ellipsoid formula. IPSS, QoL score, and Qmax, which were evaluated at 3 months after surgical treatment, were estimated for postoperative outcomes.
The end point of this study was the degree of improvement in IPSS at 3 months after surgical treatment, and favor group after surgical treatment for BPH was defined as patients who experienced an improvement in IPSS over the median degree of improvement in IPSS. Baseline characteristics between HoLEP and TURP group were compared using an analysis of variance for continuous variables and a chi-square test for categorical variables, and to identify predictive factors for favorable outcome after surgical treatment for BPH, univariate and multivariate logistic regression analysis were performed. Only the variables found to be significant on univariate analysis (P<0.05) were entered into multivariate analysis. A receiver operating characteristic (ROC) curve was used to determine the optimal cut-off value of the significant predictive factor which was identified through logistic regression analysis. All statistical operations were performed using IBM SPSS Statistics ver. 20.0.0 (IBM Corp., Armonk, NY, USA). A two-sided P-value of <0.05 was considered statistically significant.
RESULTS
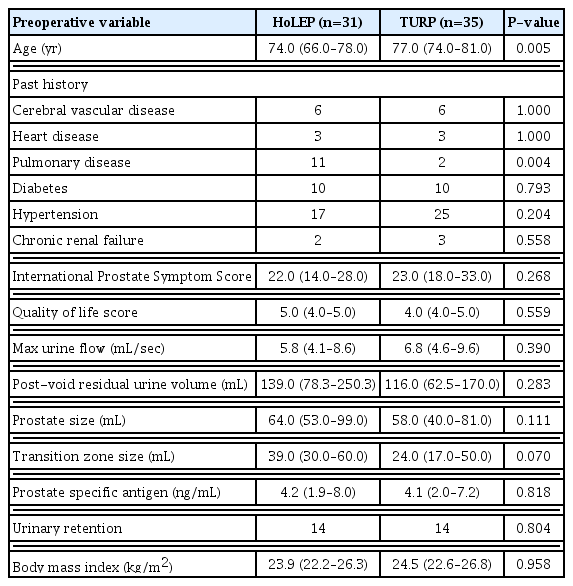
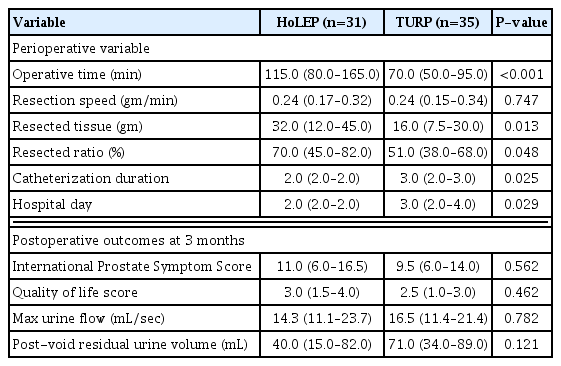
The median age of all included patients was 75.50 years (range, 70.00–79.25 years), and the median degree of improvement in the IPSS was 13.00 (range, 6.00–19.00). The baseline characteristics of HoLEP and TURP group are presented in Table 1. HoLEP was significantly superior to TURP in terms of resected volume (median, 32.0 gm vs. 16.0 gm; P=0.013), resected ratio (median, 70.0% vs. 51.0%; P=0.048), duration of catheterization (median, 2.0 days vs. 3.0 days; P=0.025), and hospital day (median, 2.0 days vs. 3.0 days; P=0.029). However, resection speed was not significantly different between the two groups (P=0.747). Operative time was significantly shorter in TURP (median, 115.0 minutes vs. 70.0 minutes; P<0.001). At 3 months after operation, there was no significant difference in urodynamic results between the two groups. Perioperative outcomes and postoperative outcomes at 3 months are presented in Table 2.
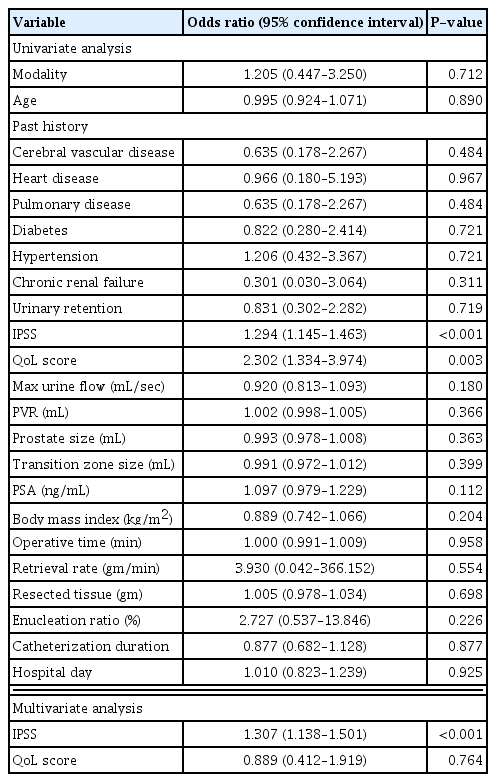
After the favorable group was defined as patients who experienced an improvement of over 13 in the IPSS, univariate and multivariate logistic regression analyses were performed to identify the predictive factors for being included in the favorable group after surgical treatment for BPH (Table 3). These analyses identified preoperative IPSS as an independent predictor of favorable outcome (odds ratio, 1.307; P<0.001). Surgical modality was not a significant predictor.
In ROC curve, preoperative IPSS 20.5 was identified as the optimal cut-off value for favorable postoperative outcome and the areas under the ROC curves was 0.887 (Fig. 1). Sensitivity and specificity were 93.8% and 67.7% in preoperative IPSS 20.5, which was identified as the optimal cut-off value, respectively.
DISCUSSION
Several authors have reported comparison studies between TURP and HoLEP [13–21]. Gilling et al. [13–15] reported outcomes at 1, 2, and 7 years after HoLEP or TURP. They demonstrated that there was no difference in postoperative urodynamic results between TURP and HOLEP. However, they reported that HoLEP was superior to TURP in duration of catheterization and the duration of hospital stay. The results of several prospective and randomized trials are reported [17–20]. Authors of prospective and randomized trials have reported that HoLEP is superior to TURP in duration of catheterization and hospital stays. In addition, they have demonstrated that TURP is superior to HoLEP in operative time. Several authors have suggested that there was no difference in postoperative urodynamic results between HoLEP and TURP [17,19], while others argue that HoLEP is slightly superior to TURP in this aspect [18,20]. Procedures in previous reports about the comparison between TURP and HoLEP were performed mostly by experts who have extensive experience of transurethral surgery. To the best of our knowledge, there is no comparative study of learning curves between TURP and HoLEP. For this reason, the predictive factor that is useful for young beginner urologists who agonize about selecting a surgical modality before performing surgical treatment for BPH should be identified.
Preoperative IPSS has been known as one of the predictors for favorable outcome in BPH patients who were treated using TURP [22–24]. Chuang et al. [23] and Hakenberg et al. [24] reported that patients showing severe preoperative IPSS obtained a greater improvement in postoperative IPSS than patients showing mild preoperative IPSS. A preoperative IPSS value of 17 is the cut-off value for the prediction of favorable postoperative outcome [23,24]. However, preoperative IPSS was not an independent predictor of favorable outcomes after TURP in these studies because they did not perform multivariate analysis. Moreover, these studies had a limitation in that they arbitrarily defined significant symptomatic postoperative improvement as a decrease of 10 or more symptom score points. Bruskewitz et al. [22] also reported that preoperative IPSS could be one of the predictors for favorable outcome after TURP. However, they also performed a multivariate analysis.
The authors identified that preoperative IPSS was a statistically significant independent predictor for favorable outcomes after surgical treatment in BPH unlike in previous reports, and that surgical modality is not an important factor for the improvement of lower urinary tract symptoms after surgical treatment in BPH. Especially, this report can be useful for beginner urologists who do not overcome the learning curve of surgical treatment for BPH, because this study was based on the experiences of young beginner urologists.
HoLEP is known as having a steep learning curve, and several studies have reported on this subject [6–11]. By comparing outcomes in HoLEP that were performed by an unexperienced urologist and by a urologist with extensive experience with transurethral surgery, El-Hakim and Elhilali [8] suggested that extensive experience with transurethral surgery is a prerequisite for the success of HoLEP. Shah et al. [11] reported that an urologist inexperienced with HoLEP could perform the procedure with reasonable efficiency after 50 cases; their prospective study was based on the experiences of a surgeon who has performed transurethral surgery in 150 cases. Bae et al. [6] also reported that they reached a stable enucleation and a morcellation efficiency state after 30 cases and 20 cases, respectively. Meanwhile, Brunckhorst et al. [7] reported that they experienced a learning curve of 40–60 cases for the HoLEP procedure in their retrospective study, which was based on the experiences of a surgeon who performed transurethral surgery in 500 cases. A recently published report demonstrated that 20 cases are probably sufficient to give the surgeon the impetus to continue with the technique [10], and Elshal et al. [9] suggested that preoperative prostate volume, the number of previously performed cases, and case density are the main influential factors in the learning curve.
Nevertheless, the authors indicate that young beginner urologists should concentrate their attention on the severity of symptoms rather than on the selection of surgical modality when they consider surgical treatment, such as HoLEP or TURP, for patients who have lower urinary tract symptoms. In addition, since the preoperative IPSS is more of an independent predictor than the surgical modality for improvement after surgical treatment for BPH, the authors recommend that it is unnecessary to hesitate to perform HoLEP just due to its steep learning curve.
This report has the limitation that this study was designed retrospectively and the number of included patients was relatively small. However, the authors judge that the scale of this study, which was performed in 40 patients who were treated with HoLEP or TURP is sufficient for evaluating initial experience because a learning curve of 20–60 cases was shown to be necessary for learning the HoLEP procedure through previously published reports. The results that are reported in the current study need to be confirmed and validated by analyzing data from a prospective study.
In conclusion, when young and beginner urologists plan to perform surgical treatment for BPH, they should consider that the severity of symptom is the most important factor for favorable outcomes. Since the type of surgical modality for managing BPH is not an important factor, the authors suggest to young beginner urologists that it is unnecessary to hesitate to perform HoLEP due to its steep learning curve.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.