INTRODUCTION
Appendiceal mucocele is an uncommon disease of the appendix, and its incidence is assumed to account for 0.2%–0.7% of all appendectomy specimens [1,2]. It can be induced by mechanical obstruction for various reasons; but mucocele induced by mucosal prolapse of the appendix itself cannot be hardly found, to the best of our knowledge. In this report, we present the case of a 38-year-old woman who was diagnosed with appendiceal mucocele secondary to appendiceal mucosal prolapse.
CASE REPORT
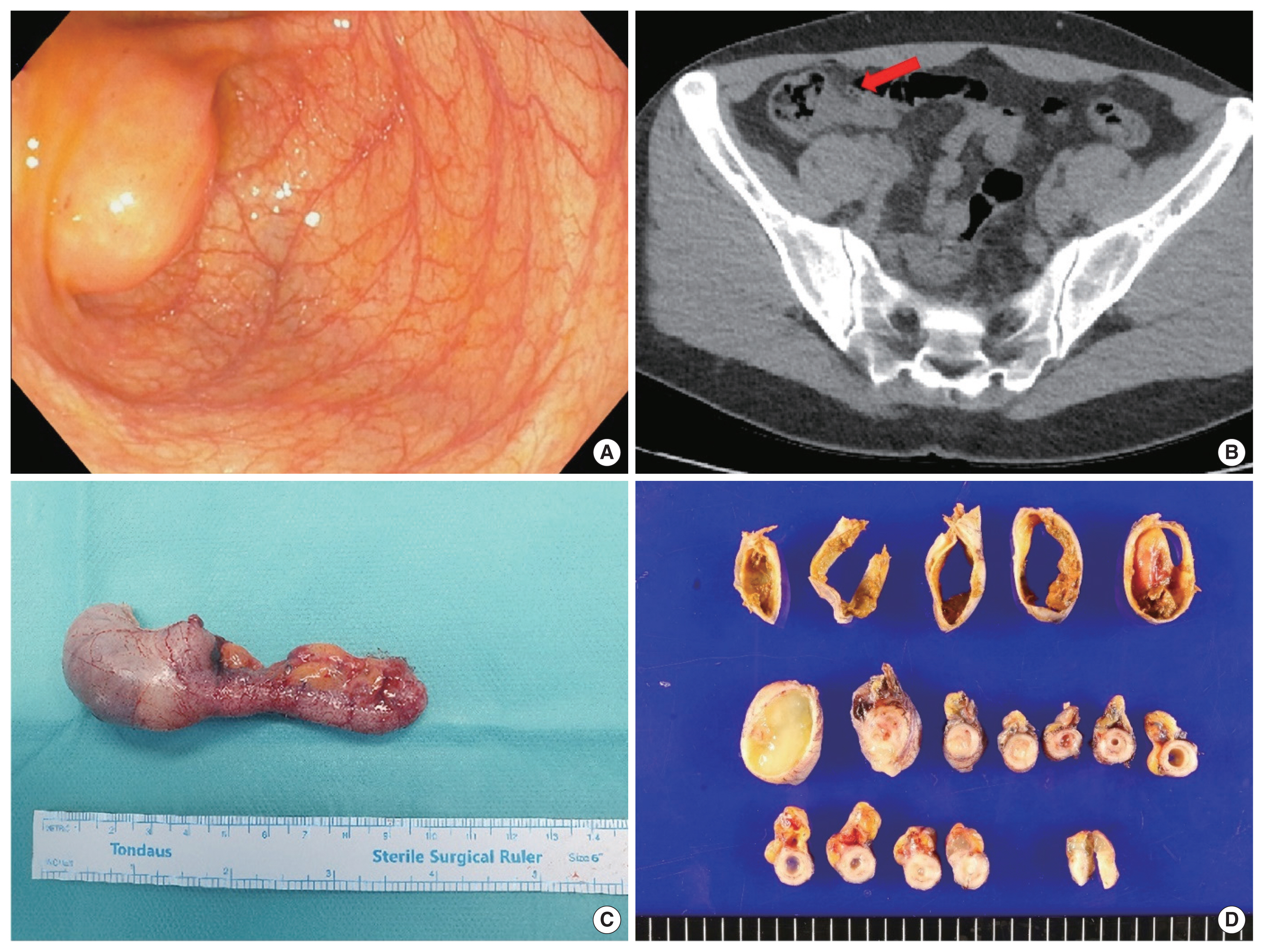
A 38-year-old woman without any specific medical history was referred from an outside hospital because of a known appendiceal mass, which was detected by a colonoscopy during a health screening program. A colonoscopy performed by an outside hospital showed an approximately 2-cm-sized subepithelial lesion with a smooth overlying mucosal surface on the base of the appendiceal orifice, suggesting a submucosal lipoma (Fig. 1A). She was asymptomatic, and no remarkable signs were noted on the physical examination of her abdomen. Initial laboratory findings were unremarkable, wherein the white blood cell count (7,300 cells/mL; normal range, 4,000–10,000 cells/mL) and C-reactive protein level (0.48 mg/dL; normal range, 0–0.5 mg/dL) were in the normal range. Contrast-enhanced abdominal computed tomography findings showed an approximately 2.5-cm-sized, thin-walled tubular cystic structure at the right lower abdomen adjacent to the appendiceal orifice, suggesting an appendiceal mucocele in the proximal portion (Fig. 1B). Laparoscopic cecal wedge resection was performed. No evidence of ascites, adhesions, mucinous implants, or pseudomyxoma peritonei was found in the abdominal cavity.
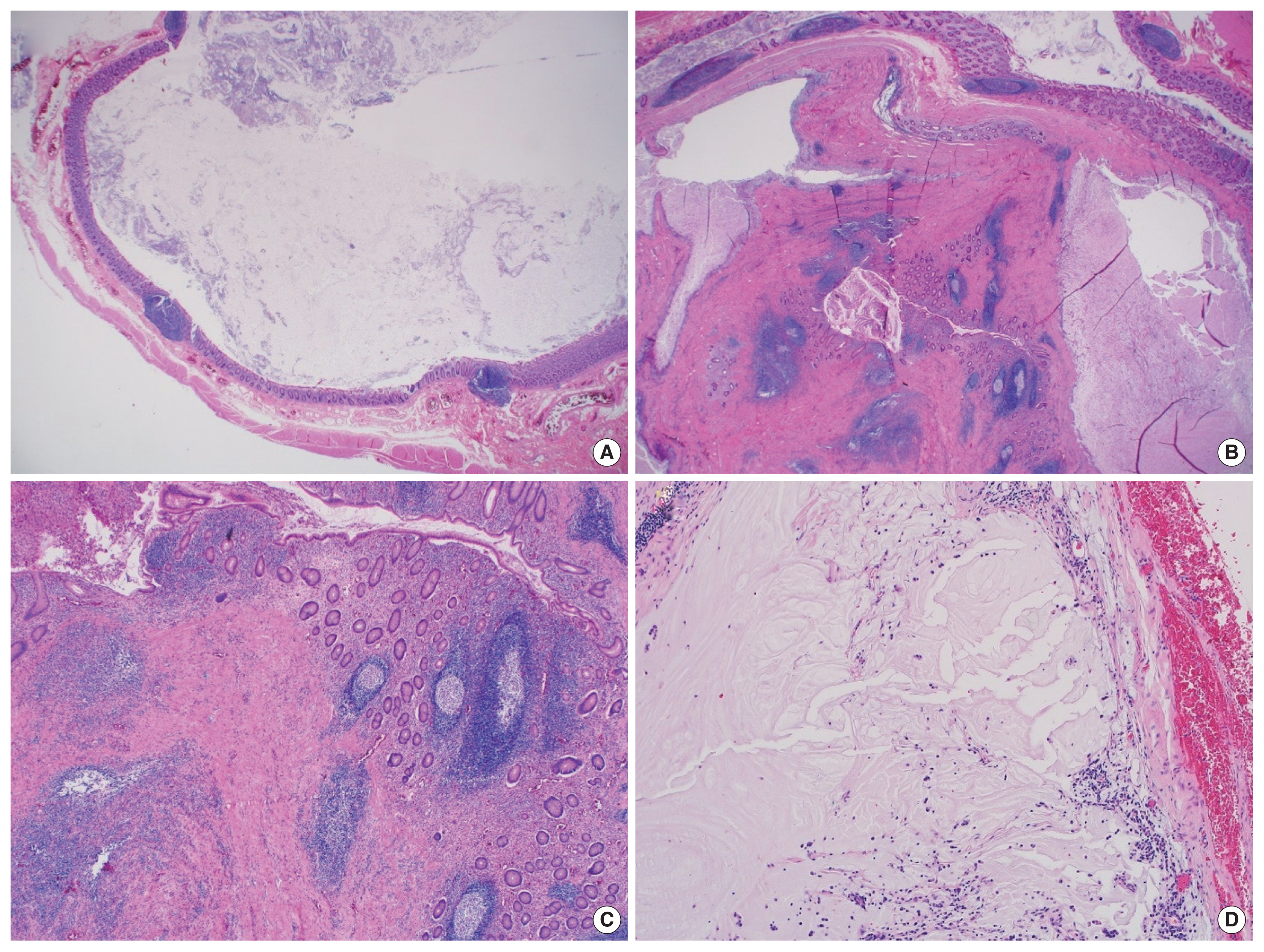
The gross appearance of the appendix revealed marked dilation of the proximal appendix, measuring 2.5 cm in diameter, and the distal portion showed relatively unremarkable findings (Fig. 1C). Multiple serial sections of the specimen revealed a dilated lumen containing white-grayish mucinous fluid at the proximal portion, a polypoid mass at the mid portion, and a slightly dilated distal portion filled with mucoid material (Fig. 1D). Microscopically, the proximal portion of the appendix showed a dilated lumen with unremarkable mucosa (Fig. 2A). A 1.5-cm-sized intraluminal polypoid mass was found in the mid portion of the appendix, which showed histologically hypertrophic features of the mucosa, such as mucosal prolapse, hypertrophic mucosal glands, presence of muscularis mucosa, entrapped or dilated mucosal crypts, and a small mucin pool (Fig. 2B, C). The adjacent appendiceal mucosa and submucosa were broadly continued with the above intraluminal mass, but no suspicious stalk-like structure of the pedunculated polyp was noted. The mucosa of the distal appendix was ulcerated, and mucin spillage without a viable lining epithelium was found in the peri-appendiceal fat tissue around the appendiceal tip (Fig. 2D). There was no evidence of neoplastic features in the entire appendix. An appendiceal mucocele associated with appendiceal mucosal prolapse was pathologically confirmed. After the operation, the patient recovered smoothly, and the patient was discharged on the second postoperative day. The patient provided written informed consent for the publication of clinical details and images.
DISCUSSION
Mucocele of the appendix refers to slow and gradual dilation of the appendix with mucin accumulation, with no signs of infection inside the organ. It can occur secondary to the inflammatory or neoplastic proliferation of the appendix mucosa or lesions adjacent to the appendiceal orifice.
In this case, apart from the appendiceal mucocele, the intraluminal mass in the middle portion of the appendix was an unusual finding. Because the mass showed no cellular atypia, the possibility of a neoplasm can be excluded. The appendix revealed no evidence of congenital abnormalities such as duplication and diverticulum, and the mass was a true intraluminal mass consisting of a mucosal component.
For the differential diagnosis, we considered hyperplastic polyps, inflammatory fibroid polyps, hamartomatous polyps, appendiceal intussusception, and hypertrophic or prolapsed mucosa of the appendix. Findings such as elongated crypts and superficial serration were not clear in the present case; therefore, it seemed to be far from those of general hyperplastic polyps. Although there was a somewhat fibrotic portion at the center of the mass, it might have been hypertrophic muscularis mucosa and admixed collagen bundles of the mucosa and submucosa. These findings differed from those of inflammatory fibroid polyps, in which the proliferation of spindle cells with various inflammatory cells was the main histological feature. Additionally, the presence of a mucin pool within the mass-like lesion did not support inflammatory fibroid polyps. Therefore, hamartomatous polyps should also be discriminated. However, there were no other remarkable polyps in the other gastrointestinal tracts, and the characteristic thick and broad bands of the muscularis mucosa centrally supporting the polyp were not histologically noted in the present case. Because acute and chronic inflammation with several mucin pool formations and reactive fibrosis with disarrayed muscularis mucosa was thought to be the main histological features of the lesion, these histological findings were reminiscent of colitis cystica profunda and solitary rectal ulcer syndrome. Indeed, the two diseases are known to show similar histological findings in the late stage. Considering the polypoid shape, haphazardly and cystically dilated benign colonic crypts in the deeper portion, and disarrayed muscularis mucosa, it is rather similar to the microscopic findings of solitary rectal ulcer syndrome. In the case of the appendix, this is also unusual; therefore, we considered referring to it as a descriptive diagnosis of hypertrophic or prolapsed mucosa.
By definition, intussusception means “portion of the bowel (intussuscipiens) swallows another length of the bowel (intussusceptum)” [3]. According to the classification of appendiceal intussusception proposed by Moschcowitz [4] in 1910 and later modified by McSwain [5] in 1941, intussusception in the mid portion of the appendix corresponds to type II or IV of appendiceal intussusception; invagination starting at some point along the length of the appendix (type II) or retrograde intussusception, where the proximal appendix is invaginated into the distal appendix (type IV) [3]. Intussusceptum generally involves the entire intestinal wall; however, this case is controversial because only the mucosa and submucosa are involved. There may be controversy as to whether mucosal and submucosal intussusception can be considered real intussusception.
Therefore, we considered the possibility of a prolapse. However, prolapse is defined as “a condition in which organs fall down or slip out of place.” Therefore, it is not a perfectly appropriate diagnosis because the mucosal mass is confined to the appendix itself without protrusion to other parts.
Kobayashi et al. [6] presented a case with a mucosal lesion of the appendix masquerading as an appendiceal neoplasm with microscopic findings similar to the present case. It has been described as an inflammatory polyp with ductal hyperplasia and stroma dilatation with smooth muscle, suggesting a mucosal prolapse syndrome (MPS)-like inflammatory polyp associated with appendiceal diverticulitis [7,8]. They also noted that these MPS-like findings by mechanical traction can be mostly observed in colonic lesions, but rarely in the, but rarely in the appendix. However, it is thought that further consideration is needed regarding the use of the term ‘MPS’ in appendiceal lesions.
For instance, in another similar condition in the rectoanal area, rectal prolapse can be classified as complete (full thickness of the rectal wall) or partial, external (protruding to the anus) or internal, and circumferential (prolapse involving the whole circumference of the wall) or segmental.
Internal rectal prolapse can be defined as a funnel-shaped infolding of the upper rectal or lower sigmoid wall that can occur during defecation [9]. Mucosal prolapse or partial rectal mucosal prolapse refers to the prolapse of loosening of the submucosal attachments to the muscularis propria of the rectal wall [10]. Most studies define mucosal prolapse as external segmental prolapse [11]. Many sources differentiate between internal rectal prolapse and mucosal prolapse, implying that the former is full-thickness prolapse of the rectal wall. Internal mucosal prolapse (or rectal internal mucosal prolapse) refers to prolapse of the mucosal layer of the rectal wall which does not protrude externally. Rectal prolapse and internal rectal intussusception have been classified according to the size of the prolapsed section of the rectum, the function of rectal mobility from the sacrum, and infolding of the rectum. This classification also considers sphincter relaxation [12].
If the concept of sliding to other organs is applied to the appendix as external, then involving the mucosal layer is applied as partial. It can be seen that this case could be diagnosed as partial and internal mucosal prolapse. However, there is no consensus on whether or not the same criteria should be applied in the appendix as those in the rectum. Accordingly, the intraluminal mass shown in this case created difficulty in making a clear diagnosis. Further discussion and agreement between pathologists are necessary.
In conclusion, we report the first case of mucosal prolapse of the appendix resulting in mucocele and review the concepts of appendiceal intussusception and prolapse.