INTRODUCTION
Mycosis fungoides (MF)-large cell transformation (LCT) is a histopathological transformation of neoplastic small lymphocytes with a clonally identical large cell phenotype and is reported in 20%–50% of cases of advanced mycosis fungoides [1]. Accurate staging is important for predicting prognosis to determine precise treatment regimens. The prognosis of MF depends on the stage, mainly the type and degree of skin involvement, as well as the presence or absence of extracutaneous findings [2].
Fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) is a non-invasive imaging technique that demonstrates metabolic assessment of normal tissues or disease states for the staging and evaluation of tumor responses in nodular-based lymphomas and solid tumors [3]. Staging with CT scans is mainly based on anatomy information. The lymph node findings in patients with MF may be underestimated and misinterpreted as a non-specific inflammatory condition such as dermatopathic lymphadenopathy [4].
CASE REPORT
1. Patient information
A 55-year-old man had a 5 cm mass in his left neck for 4–5 months. He had systemic multiple swellings, systemic psoriasis, itching, and erythematous patch plaques for 3 years. He was controlled with atrial fibrillation and congestive heart failure in the cardiology department, and there were no special findings except for a history of surgery for varicose veins in the past. This study was conducted according to the ethical guidelines of the Institutional Review Board and Ethics Committee of Soonchunhyang University Hospital, and the requirement to obtain informed consent was waived.
2. Diagnostic assessment
Laboratory findings showed lactate dehydrogenase (LDH) was above 800 U/L. A bone marrow biopsy was performed on the pelvic bone to confirm bone marrow invasion. There was no evidence of bone marrow involvement by malignant cells. Cytogenetic examination revealed no apparent cytogenetic abnormalities. Histopathological study was performed at three sites with surgical excision; left flank, scalp, and anterior neck. Mycosis fungoides was diagnosed in the left flank and scalp. Furthermore, LCT was confirmed in the anterior neck soft tissue lesion. Immunohistochemical stains showed positive for CD3, CD4, and CD30 with 30%–40% of Ki-67.
3. Fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography finding
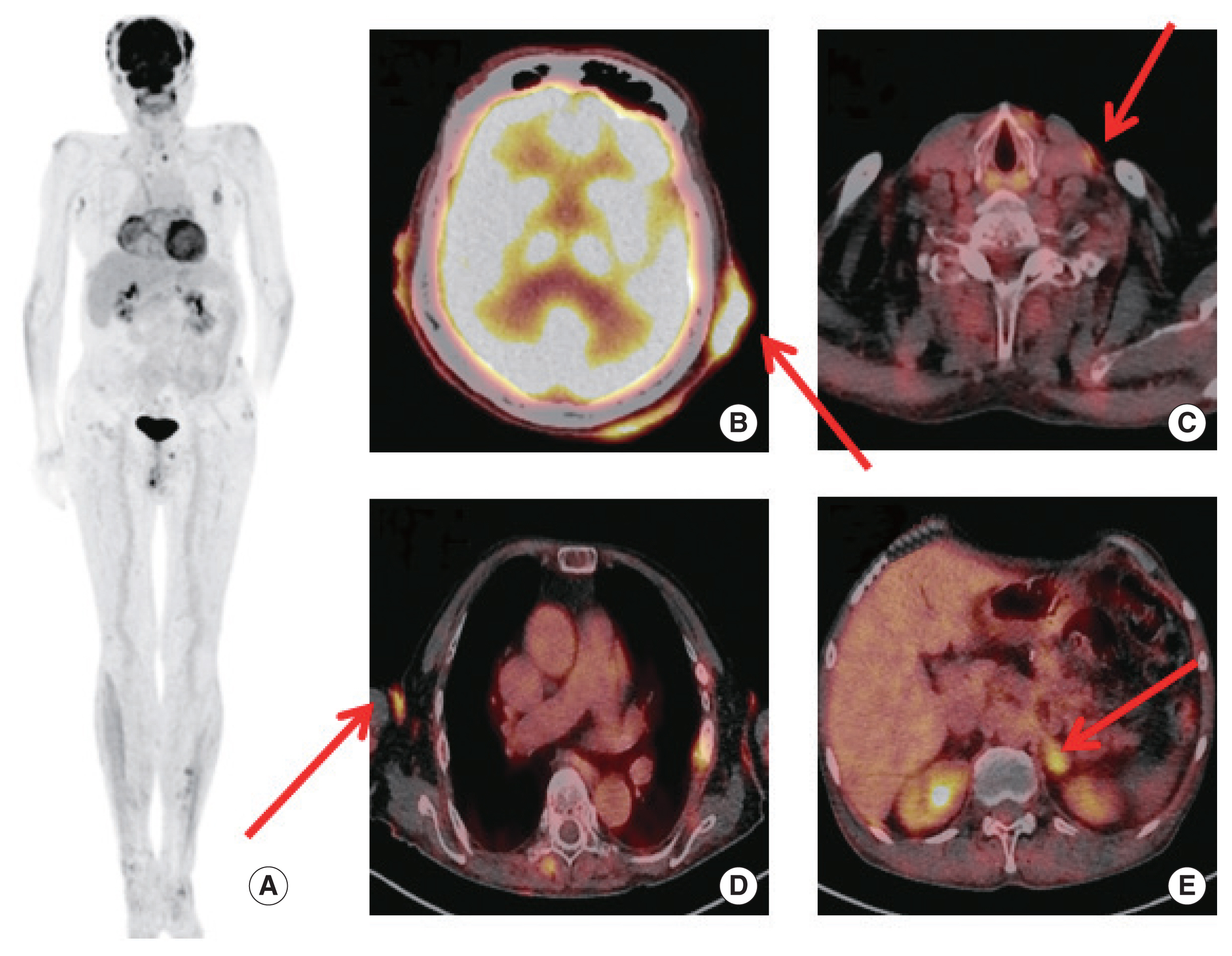
We tried the 18F-FDG PET/CT (Biograph 128mCT; Siemens Medical Solutions, Knoxville, TN, USA) scan to evaluate the number of cutaneous lesions and the presence of extracutaneous organ. The patient fasted for at least 6 hours with less than 120 mg/dL of peripheral blood glucose level. He was administered an intravenous injection of 270 MBq 1 hour prior to imaging without any intravenous contrast agent. The 18F-FDG PET/CT findings showed cutaneous hypermetabolic lesions in the scalp, anterior neck, axilla, upper thoracic back, left flank, left buttock, right inner thigh, and both heels (Fig. 1). The maximum standardized uptake value (SUVmax) of the anterior scalp was 11.0. The SUVmax of the anterior neck was 2.7, which was previously excised. There are extracutaneous lesions involving the left cervical lymph node, both inguinal lymph nodes, and the left adrenal gland (although not pathologically confirmed). The SUVmax of the left adrenal gland was 4.9.
4. Therapeutic intervention
The patient received photochemotherapy followed by 2 cycles of ProMACE-CytaBOM (prednisone, methotrexate, doxorubicin [Adriamycin], cyclophosphamide, and etoposide alternating with cytarabine, bleomycin, vincristine [oncovin], and methotrexate) as chemotherapy. On day 1, 1,175 mg of Cytoxan (650 mg/m2) and 215 mg of etoposide (120 mg/m2) were injected. For the first 7 days, 110 mg of prednisolone was taken orally. On day 8, 545 mg of cytarabine (300 mg/m2), 2 mg of vincristine (1.4 mg/m2), and 215 mg of methotrexate (120 mg/m2) were injected in the respective order. On day 9, 45 mg of leucovorin (25 mg/m2) was injected, and 110 mg of prednisolone was taken orally for another 7 days. Despite receiving two cycles of this treatment, the patient’s general condition deteriorated and the patient eventually expired.
DISCUSSION
MF is a rare type of non-Hodgkin’s lymphoma (NHL) but is the most common form of cutaneous T-cell lymphoma. Three classical clinical cutaneous phases of MF are erythematous patches, infiltrated plaques, and tumors [7]. LCT of MF is histopathologically defined as the presence of large cells (cells at least 4 times the size of small lymphocytes) that exceed 25% of the cell population. The presence of LCT often leads to a more aggressive form of the disease and in turn, worse survival. The prognostic factors for a shortened survival were stage IV, age, large-cell transformation, and increased LDH [1,8]. Treatment for MF depends on the stage of the disease. The early stages of MF are very sensitive to topical treatments such as topical chemotherapy, ultraviolet irradiation, and immunomodulators. On the other hand, systemic disease demands more aggressive and potentially more toxic therapies, such as systemic chemotherapy or whole-body skin electron beam therapy [9].
18F-FDG PET/CT is more accurate than CT alone for staging, evaluating response to therapy, and detecting disease recurrence for Hodgkin’s disease and NHL [6]. In a study involving 19 MF patients, 13 patients with local cutaneous disease, one patient with lymph node involvement, one patient with visceral involvement, and three patients with LCT were found to be positive on 18F-FDG PET/CT. The mean±standard deviation SUVmax of their LCT was 4.2±0.9, which was higher than the mean SUVmax of lymph nodes [9]. In our case, the area where the LCT appeared was the anterior neck and the SUVmax was 2.7, but underestimation may need to be considered because the image was taken after an excisional biopsy. The definitive biopsy is recommended by the International Society for Dermal Lymphoma and the Skin Lymphoma Task Force of the European Cancer Research and Treatment Organization as the preferred method for evaluating abnormal lymph nodes. Their recommendation is to select the largest peripheral lymph node of the skin area involved and/or the lymph node showing intense FDG uptake for biopsy [10].
Most studies or case reports on 18F-FDG PET/CT have been limited to MF. We report a rare case of MF-LCT involving cutaneous lesion, lymph node, and visceral metastasis. We expect the potential role of 18F-FDG PET/CT in large studies of MF-LCT.