INTRODUCTION
Carotid artery stenting (CAS) is an effective alternative to carotid endarterectomy (CEA) for the treatment of carotid stenosis. The transfemoral approach is the traditional approach in performing CAS with a high success rate. However, there are situations a transfemoral approach can not be done such as extensive atherosclerotic disease in the aortic arch, iliofemoral occlusive disease, dissection of the thoracic aorta, etc. In such a case, the transradial approach can be a useful alternative approach. We report a case of symptomatic carotid artery stenosis combined with Leriche syndrome which is an aortoiliac occlusive disease, treated by CAS by transradial approach with good result.
CASE REPORT
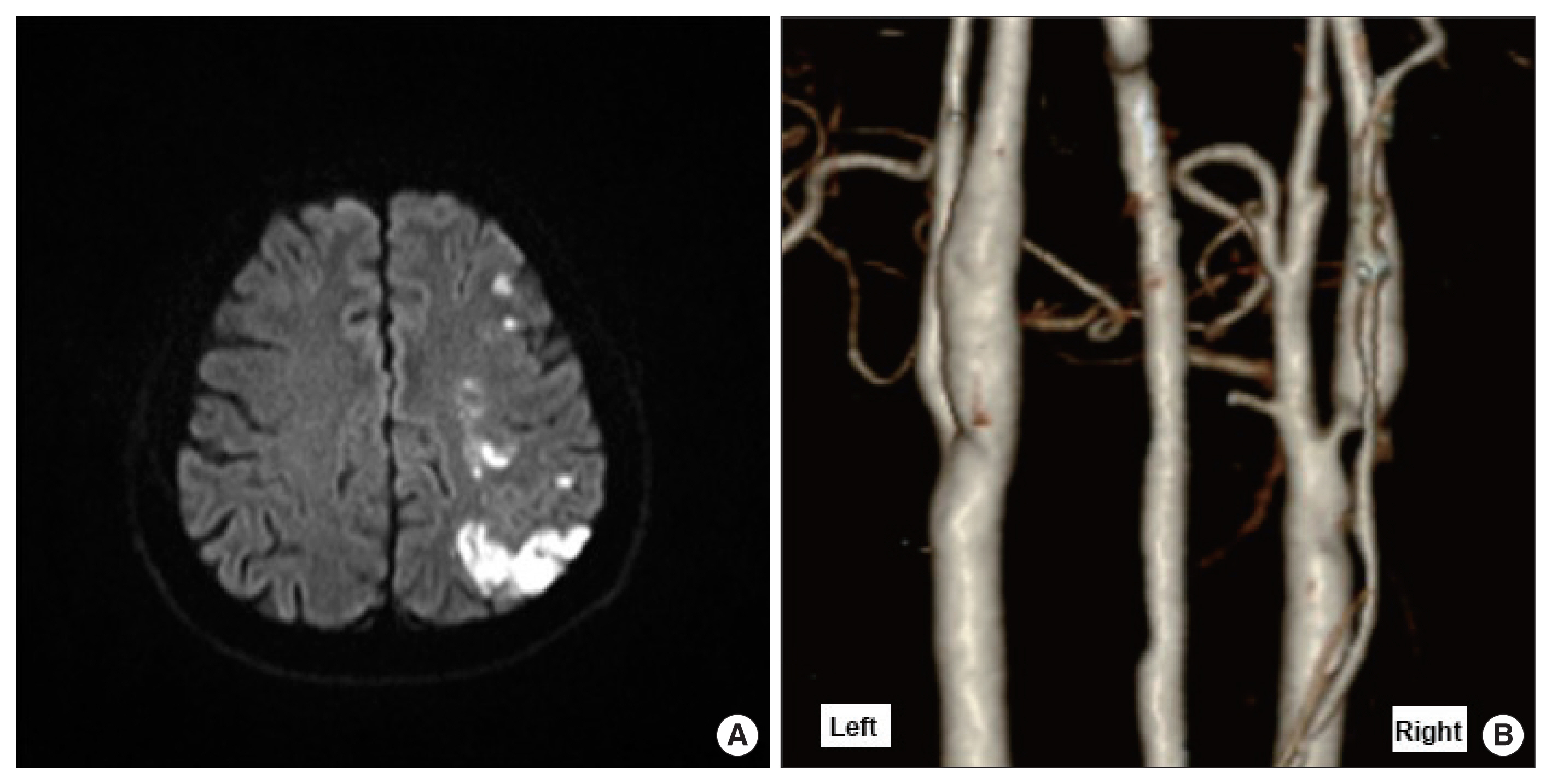
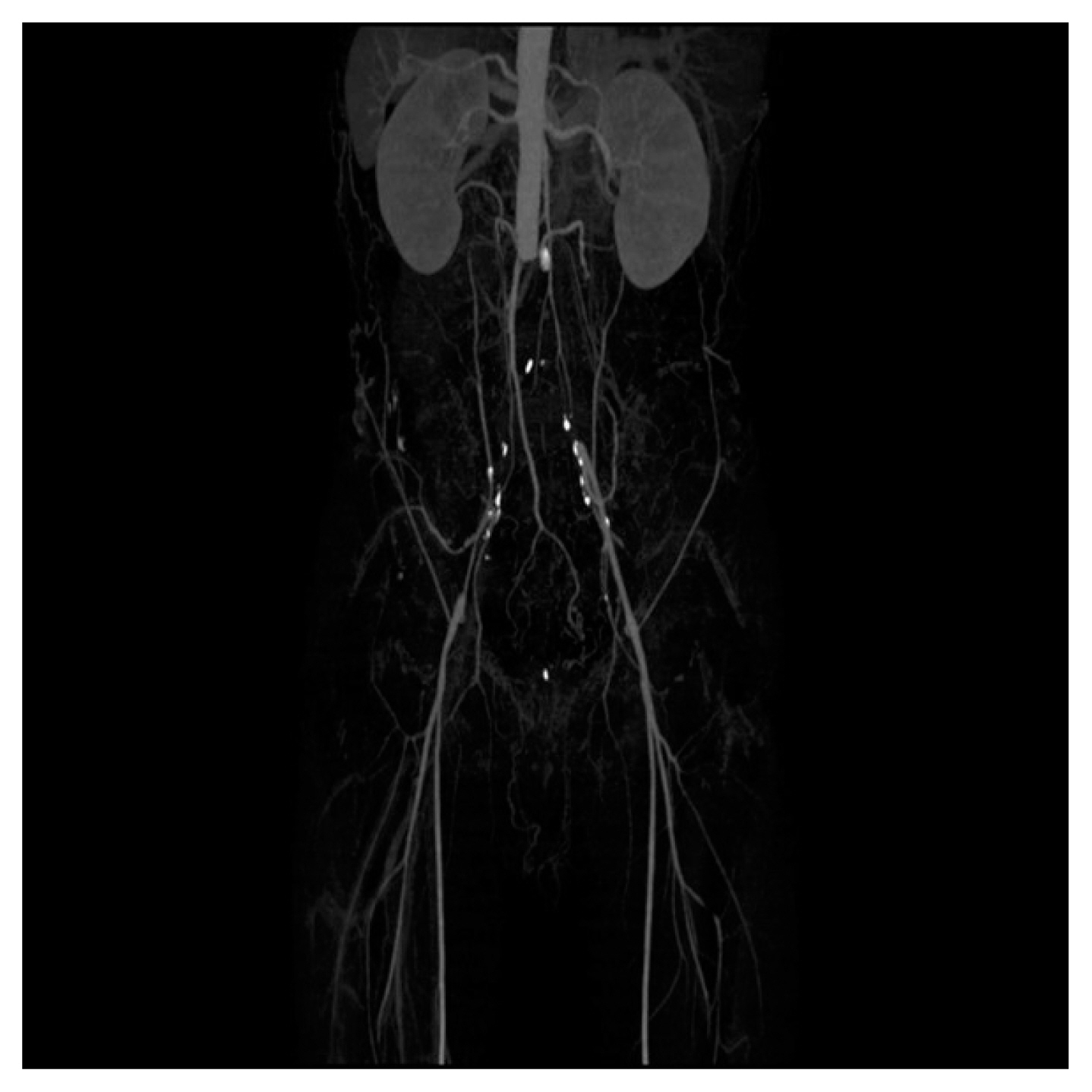
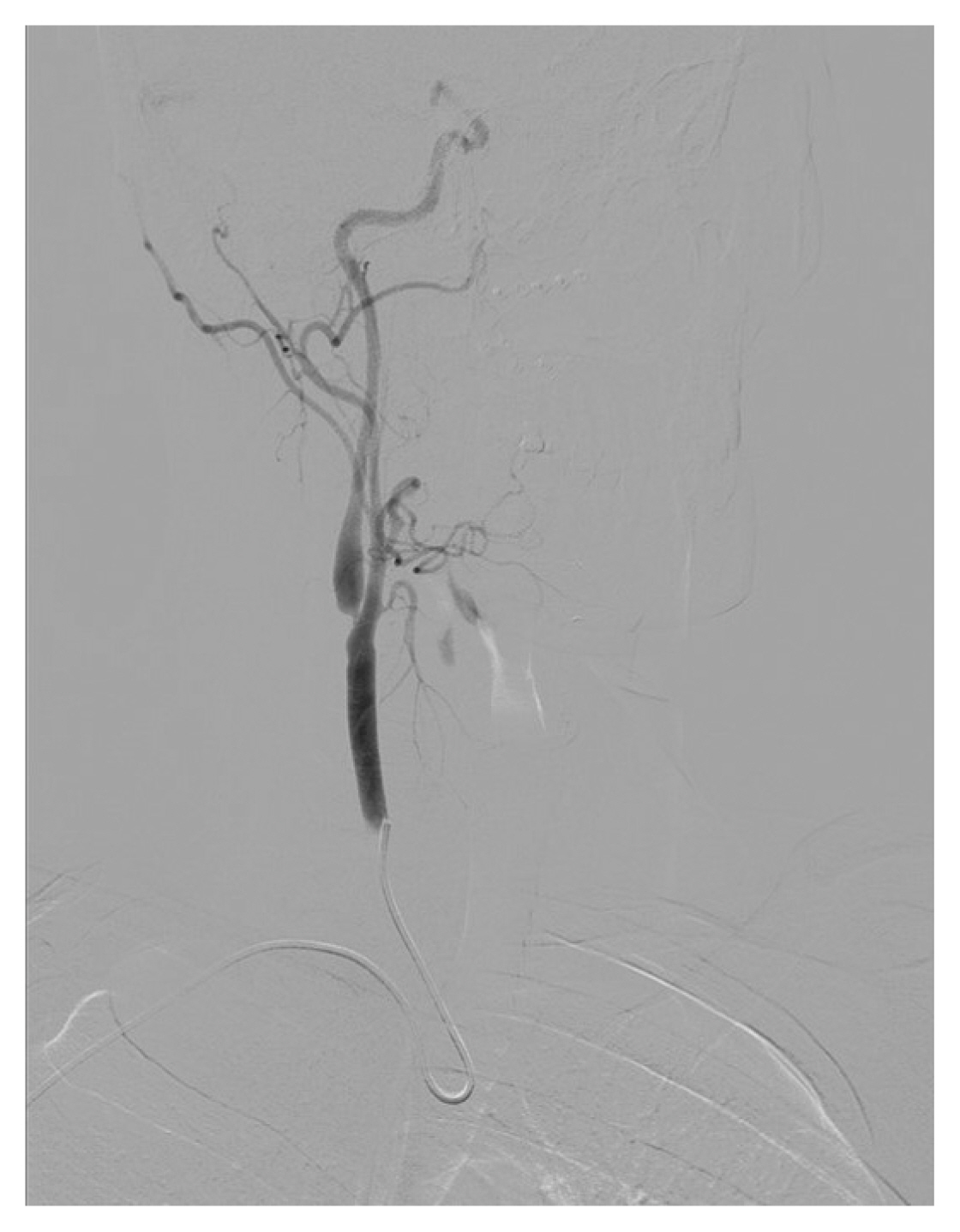
A 50-year-old male visited the emergency room of Soonchunhyang University Gumi Hospital with dysarthria and right-side weakness. The patient had a 45 pack-year smoking history and no other underlying disease. His National Institutes of Health Stroke Scale score was 3. Brain magnetic resonance imaging (Fig. 1A) showed acute cerebral infarction on left middle cerebral artery territory and carotid computed tomography (CT) angiography (Fig. 1B) revealed bilateral carotid stenosis (left carotid stenosis: 50% stenosis, right carotid stenosis: 90% based on NASCET [North American Symptomatic Carotid Endarterectomy Trial] criteria). Work up for detection of any other stroke risk factor was done, including the cardiologic evaluation and there was no other stroke risk factor besides carotid stenosis. First, the patient was on dual antiplatelet (aspirin 100 mg, clopidogrel 150 mg) medication, and hydration and neurological deficit subsided after 2 days of admission. The left carotid stenosis was symptomatic with 50% stenosis and the right carotid stenosis was asymptomatic but was severe, so both carotid stenoses were planned to be treated by CAS. The more severe right side was planned to be treated first and then the left side. Dual antiplatelets were given for about a month so no other antiplatelet loading was done. On procedure, both the femoral artery had no pulse so we could not proceed with the procedure. CT angiography of the lower extremity was done showing Leriche syndrome, an aortoiliac occlusive disease involving the blockage of the abdominal aorta as it transitions into the common iliac arteries (Fig. 2). It seemed difficult to perform CAS because the usual and familiar femoral access was not available, so we planned CEA. But the patient strongly insisted on CAS and we finally planned CAS through a radial approach. Allen’s test was negative, and we punctured the right radial artery and the 5F arterial sheath was inserted and then switched to 7F and 8F sheath sequentially not to rupture of the small radial artery by the 8F sheath we planned to use (Fig. 3). Verapamil (2.5 mg) and nitroglycerine (200 μg) were injected via arterial sheath in a radial artery to prevent arterial spasm, and 3,000 unit of heparin were given intravenously to match ACT of 200–300 seconds. There was an extreme angulation at the right common carotid artery (CCA) origin so Simmons catheter was used to cannulate the CCA and an angiogram was done (Fig. 4). It was difficult to advance the guiding catheter because of the extreme angulation between the brachiocephalic trunk and CCA. The guiding catheter was pushed to the CCA over the wire, and failed so the buddy wire was attempted, and failed, and finally over Simmons catheter but failed. The VISTA BRITE TIP, 8F JL 6 (Cordis Corp., Santa Clara, CA, USA) guiding catheter which is used for coronary artery stenting had a shape appropriate for a selection of CCA so it was planned to be used. It had a ‘C’ shape so we reshaped the tip using hot steam to a ‘U’ shape, a similar shape with Simmons catheter and directly cannulated the CCA with the guiding catheter using the “pullback and rotate” technique, the same technique used for Simmons catheter for selecting CCA, without difficulty (Fig. 5). A distal embolic protection device (FilterWire EZ; Boston Scientific, Marlborough, MA, USA) and Carotid WALLSTENT (Boston Scientific) were used successfully (Fig. 6). After the procedure, the patient had an asymptomatic radial artery occlusion (RAO). The left carotid stenosis was planned and we could not use the right radial artery, so the left carotid stenosis was performed via the left radial artery in the same fashion with the technique described above, uneventfully (Fig. 7).
The patient provided written informed consent for the publication of clinical details and images.
DISCUSSION
CAS is an effective alternative to CEA for the treatment of carotid stenosis. The transfemoral approach is the traditional approach in performing CAS with a high success rate. However, there are situations a transfemoral approach can not be done such as extensive atherosclerotic disease in the aortic arch, iliofemoral occlusive disease, dissection of the thoracic aorta, etc. In such a case, when a transfemoral approach is not available, transbrachial, direct transcervical, or transradial approach can be considered as alternative access [1]. Among them, the transcervical approach is more invasive because it needs a cervical incision to prevent critical access site complications.
Transbrachial approach may also be difficult to be done due to severe complications, including brachial sheath hematoma, compartment syndrome, injury to the medican nerve, and ischemia to the hand [2]. Kiemeneij et al. [3] have reported in their access study comparing transfemoral, transbrachial, and transradial approaches for coronary artery stenting that the transbrachial approach had more major access site complication than the transradial approach. Significant benefit was found in the transradial access having fewer major complications (2.0% for transfemoral, 2.3% for transbrachial, 0% for transradial) and had the same technical success rate as transfemoral and transbrachial access.
Therefore, transradial access can be considered to be the ideal alternative to the traditional transfemoral approach when there are limitations for transfemoral access. The transradial approach was first introduced in 1989 in cardiology and several large interventional cardiology studies have shown the benefit of the transradial approach over the transfemoral approach and now it has been a standard access site in the cardiology field [4]. There are several advantages of transradial access, including the low incidence of access site complications, reduced risk of major bleeding, reduced intensive care unit and hospital length of stay, and more comfortable and better tolerated by patients due to the ability to mobilize earlier post-procedure [5]. However, compared with coronary interventions, transradial access has a technical challenge in the neurointervention field. Selection of the CCA by the radial access will be a difficult task due to the extreme angulation of the common carotid artery at the takeoff point. Despite the advantages of radial access proved in the cardiology field, technical problems made reluctant to switch from femoral to radial access, but there are increasing reports of great success by radial approach for neurointervention procedures [4].
A meta-analysis of seven eligible studies of the radial approach for CAS reported a procedural success rate of 90.8% [4]. However, this rate of success is lower than the success rate by femoral access. Tokuda et al. [6] reported a success rate of 99.5% and Shen et al. [7] reported a success rate of 96.2% for patients with type III aortic arch and 100% for type I/II arches by femoral access.
Interestingly, Gao et al. [8] included only patients with type III and bovine arch and reported a transradial success rate of 100% and a transfemoral success rate of 90%. These reports suggest that the overall success rate of femoral access is higher than radial access, but in patients with unfavorable aortic arch morphology for femoral access, such as type III and bovine arches, transradial access can be a better option. Thus, radial access is a complementing rather than competing with the femoral artery approach.
Reports of the complication rate by radial approach are not high. In a systemic review of the literature of transradial approach for neurointervention in 1,342 cases, complications related to the radial approach was classified into minor (asymptomatic and found on routine follow-up or minimally symptomatic, not requiring readmission and intervention) and major (symptomatic and require further intervention). There were two patients (0.15%) with a major complication, one patient of symptomatic radial artery occlusion, one patient of large hematoma requiring transfusion, and 37 patients (2.75%) with minor complications, including 27 patients of asymptomatic RAO, severe radial artery spasm in four patients, and small forearm hematoma in six patients [9]. Allen’s test is crucial before transradial approach to prevent major complications of symptomatic RAO. Kuhn et al. [4] reported a distal radial artery access which is a radial approach done distally in the anatomical snuffbox to lower risk of symptomatic RAO. The site of the arteriotomy is distal to the origin of the superficial palmar arch, so even if the access site occludes, the risk of ischemic symptoms will below.
A multicenter prospective randomized study by Ruzsa et al. [10] reported a crossover rate of 10% in the radial approach and 1.5% in the femoral approach. There are some contributing factors to the higher crossover rate in the radial access. First, the radial artery has a smaller caliber and arterial spasm occurs frequently making further procedure impossible. So, it is important to inject a spasmolytic ‘cocktail’ of 200 μg nitroglycerine and 2.5 mg of verapamil to prevent vasospasm of the radial artery. Second, inability to cannulate the CCA which has an extreme angulation at its origin. There are some reported techniques to overcome this problem. First, the “telescoping technique”; after engagement of CCA by the Simmons catheter using “pullback and rotate” technique, slowly advance the guiding catheter over the Simmons catheter to CCA. Second, the “retrograde engagement technique”; the guidewire is pushed and creates a loop by the aortic cusp and then engaged in the CCA in a retrograde fashion, and the guiding catheter is advanced over the wire in the same loop fashion inside the CCA.
In our case, we did not use the above techniques. Instead, a guiding catheter, VISTA BRITE TIP (Cordis Corp.) which is used for coronary artery stenting, with a shape of “C” was used. We shaped the tip of the guiding catheter with hot steam to a shape of “U”, similar shape to the Simmons catheter to be a shape appropriate for selecting the ostium of CCA and directly selected the CCA with the same technique, “pullback and rotate” used for Simmons catheter. The procedure was simple and there was no difficulty.
In conclusion, CAS is an effective alternative to CEA for the treatment of carotid stenosis. The transfemoral approach is the traditional approach in performing CAS with a high success rate. However, there are situations transfemoral approach can not be done. In such a case, a transradial approach can be a useful alternative approach. We report a case of symptomatic carotid artery stenosis combined with Leriche syndrome which is an aortoiliac occlusive disease, treated by CAS by transradial approach with good result.