SMS 2011 December;17(2):115-117.
Published online 2011 December 30 |
| Copyright ⓒ 2010 Soonchunhyang Medical Science
|
| Acute Esophageal Necrosis Associated with Esophageal Foreign Body Injury and the Development of Pneumomediastinum |
| Mi Na Kim1, Yong Kang Lee1, A Ra Choi1, Yoon Hea Park1, Dowhan Kim2, Yong Chan Lee1,3, Hyuk Lee1,3
|
| Departments of 1Internal Medicine and 2Pathology, 3Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea |
| Corresponding Author: Hyuk Lee , Tel: +82-2-2228-1978 , Fax: +82-2-393-6884 , Email: leehyuk@yuhs.ac
|

|
ABSTRACT
|

|
|
| A 74-year-old woman complained of dysphagia and hemoptysis after ingesting a fragment of crab shell while eating crab saltedfermented fish products, and presented dyspnea that had lasted for three days. Computed tomography indicated pneumomediastinum. Laboratory results revealed acute renal failure. The patient experienced respiratory distress and shock over the days following her initial presentation. Upper gastrointestinal endoscopy revealed black pigmentation of the esophageal mucosa from the middle to lower esophagus. Despite intensive care, the patient’s condition deteriorated and she died. This is the first case of acute esophageal necrosis associated with esophageal foreign body injury and the development of pneumomediastinum reported in Korea. |
|
Keywords: Acute esophageal necrosis; Foreign body injury; Endoscopy; Pneumomediastinum |
|

|
INTRODUCTION
|

|
|
| Acute esophageal necrosis (AEN) is a rare condition characterized by endoscopic findings of dark esophageal discoloration that abruptly stops at the gastroesophageal junction
[1-3]
. The reported incidence of AEN is very low, ranging from 0.0125 to 0.2%
[4,5]
. The precise etiology of AEN is unknown, but the condition appears most often to arise from ischemia, viral infection, trauma, or corrosive injury [4,6,7]. The most common clinical presentation is upper gastrointestinal bleeding
[8,9]
. The prognosis of AEN is variable, and depends on the underlying illness
[1]
. We describe a case of AEN associated with pneumomediastinum that was caused by esophageal injury. |

|
CASE REPORT
|

|
|
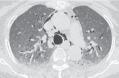
A 74-year-old woman complained of dysphagia and hemoptysis after ingesting a fragment of crab shell while eating crab saltedfermented fish products and presented to our department with dyspnea that had lasted for three days. The patient had a history of diabetes mellitus and hypertension. Upon admission to our hospital, she was afebrile, with a regular pulse of 99 bpm, a blood pressure of 160/70 mmHg, and a respiratory rate of 20 breaths/min. She suffered from dyspnea, but O2 saturation was sustained over 95% with 4 L of O2 administered by nasal cannula. The digital rectal examination was negative for blood. A test irrigation with normal saline via a nasogastric tube was also negative for blood. Non contrast-enhanced computed tomography revealed extensive pneumomediastinum but no definite esophageal injury site
(Fig.1)
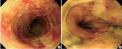
. The patient’s laboratory values included white blood cell count 6,560/μL (neutrophils 84.1%), hemoglobin 13.4 g/dL, platelets 219,000/μL, blood urea nitrogen 106.5 mg/dL, creatinine 8.97 mg/dL, total bilirubin 6.1 mg/dL, sodium 124 mmol/L, and potassium 4.1 mmol/L. Laboratory investigation revealed acute renal failure. The patient was transferred to the intensive care unit and started continuous renal replacement therapy. On day 3, the patient suffered severe dyspnea and desaturated and was connected to mechanical ventilation. Endoscopy revealed black pigmentation of the esophageal mucosa with a friable hemorrhagic area covered with yellowish exudate from the mid to distal esophagus. There was no evidence of perforation throughout esophagus (Fig. 2A). The black pigmentation of the mucosa ended sharply at the gastro-esophageal junction (Fig. 2B). An esophageal biopsy indicated an ulcer and necroinflammatory exudate
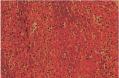
(Fig.3)
. Periodic acid-Schiff staining revealed no identifiable fungal hyphae. Immunohistochemical staining for cytomegalovirus was negative.
Despite intensive care, the patient remained hemodynamically unstable and required the administration of vasoactive agents. Her condition deteriorated over the following days. She went into multisystem organ failure and died from septic shock. |

|
DISCUSSION
|

|
|
AEN, also known as black esophagus, is a rare condition
[1-3]
. It was first described by Goldenberg et al.
[10]
in 1990. The reported incidence of AEN is very low, ranging from 0.01 to 0.2%
[5]
. The most common clinical manifestation of AEN is upper gastrointestinal bleeding, but other common symptoms are epigastric pain or burning, dysphagia, and vomiting
[4,5,11]
. Malignant melanoma, acanthosis nigricans, pseudomelanosis, melanosis, coal dust deposition, and corrosive ingestion are conditions that should also be considered in differential diagnosis [9,12].
The pathogenesis of AEN appears to be multifactorial, and ischemia is the most likely cause
[11]
. The most frequent involved location of AEN is the distal third of the esophagus, which is less vascularized than the proximal and middle esophagus [6,9,13]. AEN is associated with multiple medical conditions including renal insufficiency, diabetes mellitus, cardiovascular disease, hemodyna-mic compromise, hypoxemia, gastric outlet obstruction, alcohol ingestion, malnutrition, and trauma [6,8,14,15].
In our case, esophageal foreign body injury causing pneumomediastinum seems to have played an important role in selective esophageal ischemia. Most such foreign bodies will pass spontaneously without causing any complications. However, complications secondary to sharp esophageal foreign body injury have been reported such as esophageal perforation, fistulae, and pleural empyema
[16]
. Pneumomediastinum is normally complicated by either esophageal or pulmonary rupture, and esophageal rupture can occur as a result of foreign bodies or trauma in the system
[17]
. In a previous retrospective AEN case series, the most serious complications reported were mediastinitis and pneumomediastinum
[1]
. Our patient also had risk factors including old age, diabetes mellitus, prolonged hypotension and sepsis.
Several viral or fungal infections such as cytomegalovirus and Candida albicans can cause AEN [8,11,18]. However, immunohistochemical staining for cytomegalovirus and Periodic acid-Schiff staining for fungal infections were negative in our case.
The treatment of AEN is supportive, including adequate hydration and the use of proton pump inhibitors in most cases. Treatment should also address any comorbidities.
The prognosis of AEN patients is variable and depends on underlying clinical conditions. Deaths secondary to AEN occur in less than 6% of cases
[9]
.
In conclusion, we present the first case of AEN associated with esophageal foreign body injury and the development of pneumomediastinum in Korea. |
|

|
FIGURES
|

|
|
|
Fig.1
Computed tomography (CT) image of the patient. Extensive pneumomediastinum was noted. |

|
|
Fig.2
Endoscopic findings of the esophagus. (A) Black pigmentation of the mucosa was noted from the middle to the lower esophagus. (B) Black pigmentation of the mucosa ended sharply at the gastroesophageal junction. |

|
|
Fig.3
Microscopic findings. Biopsied mucosa from the distal esophagus shows necrotic tissue and necroinflammatory exudate (H&E, ×200). |

|
|
| |

|
REFERENCE
|

|
|
|
1.
|
Augusto F, Fernandes V, Cremers MI, Oliveira AP, Lobato C, Alves AL, et al. Acute necrotizing esophagitis: a large retrospective case series. Endoscopy 2004;36:411-5. |
|
2.
|
Burtally A, Gregoire P. Acute esophageal necrosis and low-flow state. Can J Gastroenterol 2007;21:245-7. |
|
3.
|
Singh D, Singh R, Laya AS. Acute esophageal necrosis: a case series of five patients presenting with “Black esophagus”. Indian J Gastroenterol 2011;30:41-5. |
|
4.
|
Ben Soussan E, Savoye G, Hochain P, Herv? S, Antonietti M, Lemoine F, et al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc 2002;56:213-7. |
|
5.
|
Moret? M, Ojembarrena E, Zaballa M, T?nago JG, Ib?nez S. Idiopathic acute esophageal necrosis: not necessarily a terminal event. Endoscopy 1993;25:534-8. |
|
6.
|
Hong JW, Kim SU, Park HN, Seo JH, Lee YC, Kim H. Black esophagus associated with alcohol abuse. Gut Liver 2008;2:133-5. |
|
7.
|
Reichart M, Busch OR, Bruno MJ, Van Lanschot JJ. Black esophagus: a view in the dark. Dis Esophagus 2000;13:311-3. |
|
8.
|
Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol 2007;42:29-38. |
|
9.
|
Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol 2010;16:3219-25. |
|
10.
|
Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology 1990;98:493-6. |
|
11.
|
McLaughlin CW, Person TD, Denlinger CE. Management of acute esophageal necrosis syndrome. J Thorac Cardiovasc Surg 2011;141:e23-4. |
|
12.
|
Grudell AB, Mueller PS, Viggiano TR. Black esophagus: report of six cases and review of the literature, 1963-2003. Dis Esophagus 2006;19:105-10. |
|
13.
|
Park JH, Kim HC, Chung JW, Jae HJ, Park JH. Transcatheter arterial embolization of arterial esophageal bleeding with the use of N-butyl cyanoacrylate. Korean J Radiol 2009;10:361-5. |
|
14.
|
Neumann DA 2nd, Francis DL, Baron TH. Proximal black esophagus: a case report and review of the literature. Gastrointest Endosc 2009;70:180-1. |
|
15.
|
Daniel G, Charles MN, Lawrence JB. Clinical features and out comes of acute necrotizing esophagitis (Black esophagus). Am J Gastroenterol 2000; 95:2420. |
|
16.
|
Athanassiadi K, Gerazounis M, Metaxas E, Kalantzi N. Management of esophageal foreign bodies: a retrospective review of 400 cases. Eur J Cardiothorac Surg 2002;21:653-6. |
|
17.
|
Liang SG, Ooka F, Santo A, Kaibara M. Pneumomediastinum following esophageal rupture associated with hyperemesis gravidarum. J Obstet Gynaecol Res 2002;28:172-5. |
|
18.
|
Cattan P, Cuillerier E, Cellier C, Carnot F, Landi B, Dusoleil A, et al. Black esophagus associated with herpes esophagitis. Gastrointest Endosc 1999; 49:105-7. |
|
|
|