INTRODUCTION
Myocardial ischemia in the pediatric population is rare and usually due to congenital heart disease, Kawasaki disease, or extracardiac conditions leading to poor coronary perfusion. Vasospastic angina is also a very rare disease in children and adolescents. Studies in adults suggest that Prinzmetal angina may accompany Raynaud’s phenomenon and as a complication of acute myocarditis. We report an unusual case of coronary artery vasospasm complicating acute myocarditis in an adolescent with a medical history of Raynaud’s phenomenon, with a view to increasing awareness of this possibility.
CASE REPORT
A 13-year-old boy presented with acute onset of persistent left-sided chest pain radiating to the back for 2 hours after a nap. Five days previously, he had an intermittent fever and a productive cough after school sports day. Additionally, he had a history of Raynaud’s phenomenon diagnosed 2 years ago. However, he had no medical history of obesity, cardiovascular disease, congenital heart disease, or of previous travel.
Upon arrival, the patient’s cardiac examination revealed regular heart beat without murmur and there is no jugular venous distention. The respiratory examination revealed no coarse crackles over the lung fields. His vital signs included a heart rate of 125 beats/min, blood pressure of 130/90 mm Hg, respiratory rate of 20 breaths/min, pulse oximetry of 98% on room air, and body temperature of 38.4°C.
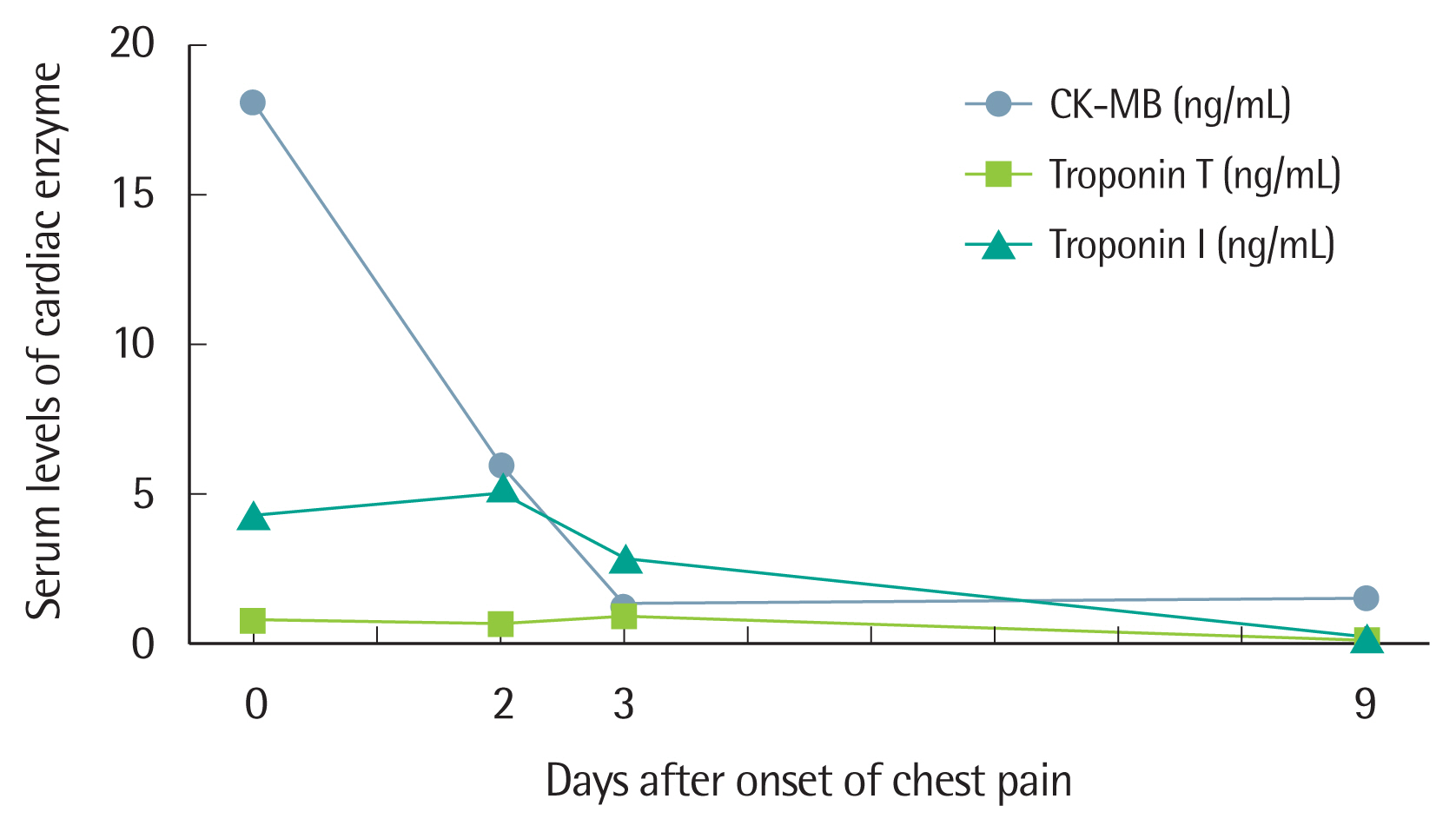
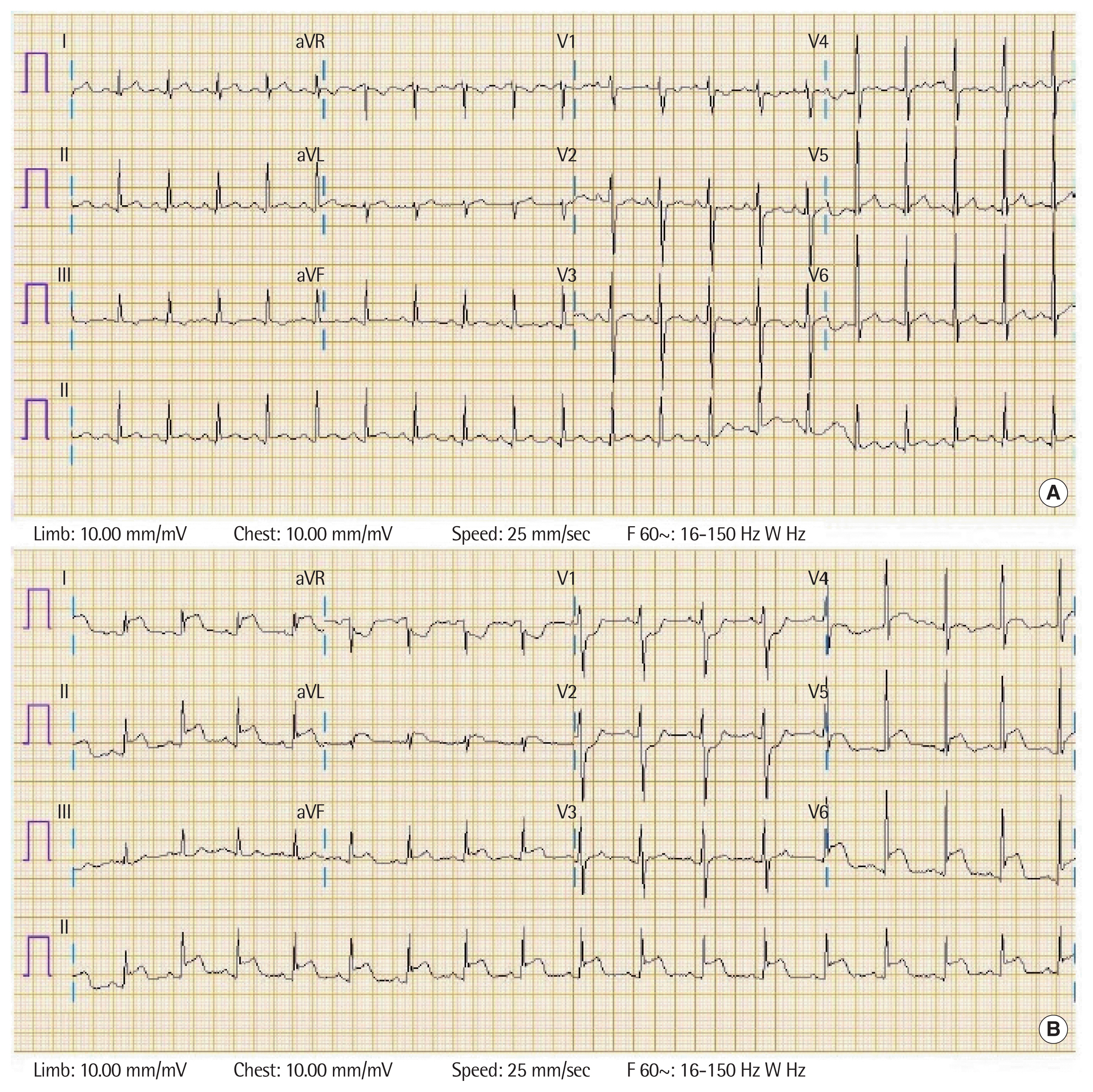
He was found to have elevated serum cardiac markers (Fig. 1) and no ST-T change on electrocardiography (ECG) (Fig. 2A) in the emergency department initially. He was admitted to the intensive care unit for suspected acute myocarditis. About 6 hours after first symptom onset, he was found to have similar findings on the ECG and elevated serum cardiac enzyme levels (Fig. 1). A chest X-ray image showed no cardiomegaly. An echocardiogram demonstrated a structurally normal heart and an absence of significant wall motion abnormality. Other laboratory findings included a white blood cell count of 6.07×103/μL (with 88% neutrophils, 6.4% lymphocytes, and 5.3% monocytes), hemoglobin level of 12.7 g/dL, C-reactive protein level of 17.63 mg/dL (reference, <0.5 mg/dL), erythrocyte sedimentation rate of 84 mm/hr (reference, <22 mm/hr), and N-terminal pro B-type natriuretic peptide level of 1,128 pg/mL (reference, <84 pg/mL). Viral serology, mycoplasma pneumoniae antibody, and antibodies for autoimmune disease were all negative.
Three hours after arriving at the emergency room, he began treating with high-dose intravenous gamma-globulin, 2 g/kg, over 24 hours, addition to antibiotics therapy with ampicillin-sulbactam, cefotaxime and azithromycin. Approximately 12 hours after the first episode, he experienced a second episode of similar chest pain, and was found to have an abnormal ECG with ST-segment elevation in the posterolateral leads that had not been seen before (Fig. 2B). We decided to perform coronary computed tomography (CT) angiography to differentiate ST-segment elevation myocardial infarction or other combined coronary vessel anomalies. Emergent coronary CT angiography demonstrated normal coronary arteries without abnormal structures, narrowing, or tearing and mildly decreased contractility of the left ventricle.
The chest pain subsided with non-steroidal anti-inflammatory drugs and nitrates after 2 hours with normalization of the ECG. On the third day of hospitalization, amlodipine was started to avoid angina attack. He was discharged 9 days later on amlodipine 5 mg once daily with the recommendation of restricting physical activity. Serum cardiac enzyme and other laboratory findings including C-reactive protein had normalized when he was discharged.
The patient provided written informed consent for the publication of clinical details and images.
DISCUSSION
According to the Coronary Vasomotion Disorders International Study Group (COVADIS), there are three core elements that establish the diagnosis of Prinzmetal angina: nitrate-responsive angina, transient ischemic ECG changes in the absence of obvious causes for increased myocardial oxygen demand, and angiographic evidence of coronary artery spasm [1]. Prinzmetal angina is caused by focal or diffuse spasm of an epicardial coronary artery, resulting in a high-grade obstruction. The pathogenesis of the coronary vasospasm is most likely related to vascular smooth muscle hyper-reactivity, increased tension of the autonomic nervous system or oxidative stress, endothelial dysfunction, and associated microvascular dysfunction [2]. Additionally, inflammatory mediators play an important role in the pathogenesis of coronary spasm. Kounis and Zavras [3] introduced the concept of “allergic angina”. On the basis of these mechanisms, several studies have suggested that there may be similarities in the pathogenesis of Raynaud’s phenomenon and coronary artery vasospasm [4,5].
In the pediatric population, anginal chest pain may occur rarely due to coronary vasospasm as a complication of acute myocarditis [6]. Coronary angiography, which is not easy to perform in adolescents, is replaced by coronary CT angiography with curved multiplanar reformatted images. The high negative predictive value of normal coronary CT results can be used to effectively exclude significant coronary artery disease and to avoid further imaging tests or catheter coronary angiography in adolescents [7].
Patients with myocarditis can be asymptomatic or present with chest pain and other symptoms. Troponin I elevation has high specificity in supporting the diagnosis, especially in conjunction with strong clinical suspicion. ECG abnormalities accompanying cardiac enzyme level elevation in the appropriate clinical setting are highly suggestive of myocarditis and are reported in up to 90% of cases [8]. The most characteristic ECG findings in differentiating myocarditis from acute myocardial infarction are diffuse ST-segment changes and resolution of the T-wave abnormality in the final stage. Assuming that both diseases occur together, symptoms of chest pain in patients with viral myocarditis may be caused by coronary vasospasm, as a result of myocarditis-induced coronary endothelial dysfunction. ECG changes during an attack and the extent of coronary artery vasospasm may predict the type and severity of any accompanying arrhythmia. Bradyarrhythmias are found to be more common in cases of inferior ST segment elevation, ventricular arrhythmias in anterior ST elevation [9], and lethal arrhythmias, such as ventricular fibrillation and advanced heart block are usually seen in cases of multivessel spasm [10]. In the case of our patient, ST elevation was recorded in posterolateral leads without dysrhythmias. Therefore, serial ECG testing and diligent interpretation is required.
Our case highlights the fact that pediatricians should be aware of chest pain due to coronary vasospasm complicating acute myocarditis. An early evaluation and active treatment should be undertaken in order to prevent ischemic myocardial dysfunction. In addition, it is worthy of note that Raynaud’s phenomenon can be associated with coronary artery vasospasm in the pediatric population as reported in studies on adults.